-
Content count
1,567 -
Joined
-
Last visited
-
Days Won
71
Posts posted by Alchemica
-
-
How do you modulate your serotonin system with dietary factors?
I wanted to try and address persistent issues at the most fundamental dietary level possible - amino acids, vitamins. I tried some challenge doses with tyrosine and tryptophan and the later seemed to provide the most robust improvements. I keep on top of B-vitamins but assumed tryptophan in dietary protein was going to be enough...
I've been abstinent from deleterious things for a long time now but it didn't mean health was improving. I couldn't shift a worsening phenotype of persistent emotional and mood dysregulation, cognitive decline, multiple night time awakenings and poor sleep quality, uncharacteristic uncontrollable verbal aggression (to the point of coprolalia), impulsiveness, intrusive thoughts, obsessiveness and plain dysphoria. SSRIs alone were not getting at the issue sufficiently. Diet, exercise and meaningful activity wasn't stopping the roller-coaster.Studies have found disturbances of tryptophan metabolism and their association with depression in alcoholics. Particularly, a decreased tryptophan ratio to other amino acids competing with tryptophan for brain entry has been investigated - diminished supply of tryptophan would lead to serotonin deficiency and thus contribute to depression in alcoholics
Depressed alcoholics had significantly decreased ratios of plasma tryptophan to amino acids sharing with it the same transport carrier into the brain (tryptophan ratio). This ratio has been shown to predict the brain serotonin concentration. It is not presently known whether amino acid modifications disappear after a period of abstinence or persist [1]. Patients who had exhibited violent behavior were observed to have tryptophan ratios lower than patients with no history of violence.Research has demonstrated a robust response to increasing plasma Trp/LNAA ratio, stimulating a significant affective response. Unexpectedly Trp supplementation not only improved central serotonergic functioning but improved the profile of tryptophan metabolism [2].
[1] http://grantome.com/grant/NIH/R01-AA006510-02
[2] https://patentimages.storage.googleapis.com/50/94/8b/2fef42545c61d4/WO2005049012A2.pdf
Using the amino acids is not just addressing pathology but providing some vital things:
A source of believable hope, when things feel hopeless
A source of day-to-day stability and connection to something when other sources of connection are non-existent or volatile
A sense of being in control, when things feel out of control
A secure quasi 'attachment relationship' to something when these might not elsewhere exist
A safe displacement onto healthier behaviours for residual impulsivity and craving
A placebo effect synergistic with added active effects. Placebo effects themselves can be potent medicine, as seen in many illnesses, from depression to Parkinson's.Sure it's better to find these things in other ways but it's often the most stable, permanent connection in times of illness and volatility one can find
In recovery: “Glutaminergic-Dopaminergic Optimization Complex Therapy”, has been well-researched in many clinical trials and shown to provide gentle activation of dopamine across the brain reward circuitry in abstinence. Additionally, significant increases in resting state functional connectivity have been demonstrated in human and animal models using state of the art resting state fMRI measurements [1]
Amino acid based therapies have led to:
Improved Physical and BESS (behavioural, emotional, social and spiritual) Scores
Reduced craving, relapse rates and enhanced recovery
Stress reduction lead to improved sleep, enhanced energy, and improved focus and performance, reduced appetite, loss of unwanted weight, decreased body inches, and enhanced well-being
Cognitive processing speeds were enhanced
Significant results were observed for weight loss, sugar craving reduction, appetite suppression, snack reduction, reduction of late night eating, increased energyResearch is needed regarding the potential for return of well-being in recovery by the gentle induction of “dopamine homeostasis;” balancing serotonergic, endorphinergic, cannabinergic, glutaminergic, dopaminergic mechanisms and restoring healthy brain function and connectivity.
While I'm just using simple aminos and vitamins, one such version that has been extensively researched is KB220Z which is composed of the following ingredients: 10 mg (500%) vitamin B6, 15 mg (1,033% of daily value) thiamine, 200 mcg (166%) chromium poly nicotinate, and a fixed dose of synaptose. Synaptose is a combination of amino acids and herbs. The amino acids include L-tyrosine, DL-phenylalanine, L-glutamine, and 5-hydroxytryptophan. The herbs include passionflower extract and a complex containing astragalus, arabinogalactans, N-acetylglucosamine, aloe vera, white pine bark extract, frankincense resin, Spirulina, Rhodiola
[1] https://dx.doi.org/10.1080%2F10826084.2016.1244551
What if the serotonergic dimension needs more urgent addressing?
I tried L-methylfolate 15mg/day (+B12 1mg) with slight improvements for a short time, then also added some tryptophan [1] to the diet. A few days into adding the Trp and the coprolalia waned, emotional regulation started to return. I started to get malleable non-intrusive thinking again. Mood started to improve. See what happens longer term
Folate deficiency seems to be an important contributor for the onset and progression of neuropsychiatric diseases [2]. L-methylfolate addresses
hyperhomocysteinemia, lower methylation reactions and tetrahydrobiopterin levels [3]. Brain folate abnormalities causes diminished production and availability of tetrahydrobiopterin (BH4) which is a critical cofactor for the rate-limiting enzymes involved in the synthesis of the monoamine neurotransmitters and may be targeted by L-methylfolate.
L-methylfolate should cause, in an over-simplistic framework:
-Activation of tryptophan hydroxylase initiates a cascade that leads to the synthesis of serotonin, and
-Activation of tyrosine hydroxylase initiates a cascade that leads to the synthesis of dopamine and norepinephrine[1] http://journals.sagepub.com/doi/abs/10.1177/0269881111430744
[2] https://www.ncbi.nlm.nih.gov/pubmed/25939915
[3] https://www.ncbi.nlm.nih.gov/pubmed/27068282Why L-methylfolate?
Many users find it quite effective - some users get quite rapid responses
"Within 1 day, I felt like my internal motor that had been idling along at a 5 out of 10 had been turned up to a 10 for the first time in a long time. I had more energy, clearer thoughts, happier disposition..."
"I felt better the first day. I feel like normal people feel. I have hope, motivation, freedom. I am completely happy."
"Within just days of my first dose, I could fell a huge, positive difference. My mind and speech were clearer, my anxiety was nearly unrecognizable, and I was just plain happy."
"...my lows vanished within first week on 15mg/day."
"Within one week of taking L-methylfolate, I had absolutely NO anxiety. It was so quiet in my soul that I almost felt anxiety about not having anxiety! It was foreign to me; the steady drip, drip, drip of adrenalin rushing through my system was shut off."
"Within 10 days, I felt more alive, motivated, energetic, and at peace then I had EVER felt in my life. "
15 mg eight days ago and I feel absolutely wonderful. Mood is great, anxiety has improved significantly, and I feel so peaceful. My energy level is up, and I feel hopeful and full of life again. I am so relieved and happy I could cry."
I am able to finally really smile and laugh. I have not been able to find humor in things for years.
I have more of a sense of well being
I have more serenity
I have an increased amount of time I feel better emotionally and mentallyThere is some support for the efficacy of both standard folic acid and L-methylfolate as an augmentation agent for depression [1]. The lowest dose of MTHF studied in depression to augment antidepressant treatment is 7.5 mg, roughly equivalent to 52 mg of folic acid. Synthesis of the monoamine neurotransmitters serotonin, dopamine, and norepinephrine is regulated by L-methylfolate, which can cross the blood brain barrier.
"Adjunctive L-methylfolate at 15 mg/day may constitute an effective, safe, and relatively well tolerated treatment strategy for patients with major depressive disorder who have a partial response or no response to SSRIs" [2]. It shows promise against negative symptoms in psychotic illness [3].
"Clinical improvement in depressed patients treated with an SSRI and l-methylfolate (0.5 to 1 mg) was 30 percent greater than that in matched patients treated with an SSRI only. A systematic review of controlled studies (total N = 247) concluded that folate augmentation (1 to 15 mg per day) enhanced the efficacy of conventional antidepressants."
"Does folate supplementation relieve symptoms of depression? A ten-week trial of 127 participants compared 0.5 mg/day folic acid (standard folate) augmentation of fluoxetine to placebo augmentation, and found that folic acid significantly outperformed placebo in terms of treatment response rate (38% vs. 18%) and overall improvement on the Hamilton Depression Rating Scale. However, the advantages for folic acid were not seen until ten weeks into treatment.
In a smaller trial, patients with depression or schizophrenia were given either 15 mg methylfolate (equivalent of 7.5 mg L-methylfolate) or placebo in addition to their existing medication regimen. Though hampered by a small sample size (24 depressed patients and 17 patients with schizophrenia), there was a statistically significant benefit on a general clinical outcome scale and there were trends toward a significant benefit on other outcome measures in the six-month study"
Administration of MTHF may have significant advantages over administration of folic acid to augment antidepressants in depressed patients who do not respond adequately to their antidepressant treatment. Such patients may or may not be folate deficient, may or may not have the inefficient form of the genotype. "Biomarkers associated with inflammation or metabolism (higher BMI) and genomic markers associated with L-methylfolate synthesis and metabolism may identify patients with SSRI-resistant depression who are responsive to adjunctive therapy with L-methylfolate" [4].
"Patients with schizophrenia who take daily folic acid in the form of methylfolate 15 mg together with an antipsychotic may have fewer positive symptoms (e.g. hallucinations and delusions) and fewer negative psychotic symptoms (paucity of thought, social withdrawal) and may respond more rapidly" [5]
[1] https://pro.psychcentral.com/l-methylfolate-for-depression-the-real-deal/
[2] https://www.ncbi.nlm.nih.gov/pubmed/23212058
[3] http://www.schizophreniaforum.org/news/l-methylfolate-shows-promise-against-negative-symptoms-schizophrenia
[4] https://www.ncbi.nlm.nih.gov/pubmed/24813065
[5] https://www.psychologytoday.com/us/blog/integrative-mental-health-care/201709/folate-depression-schizophrenia-and-dementiaAddressing homocysteine and potential B9/B12 deficiencies
While I keep on top of B-vitamins generally...
Stress can increase homocysteine levels (HCy). Higher levels of hostility were associated with higher levels of homocysteine [1]. People high in hostility are known to report more life stress, it is possible that homocysteine concentrations are elevated among these individuals due to increased stress [2].
Elevated levels of homocysteine have been associated with major depressive illness (and positively correlated with anger and length of depressive episode), bipolar disorder (both during manic and depressive episodes and in euthymic state) and various other mental conditions. "Studies of subjects with a wide range of cognitive functions showed increased plasma Hcy and decreased serum folate and enzymatic cofactors involved in methionine and Hcy metabolism are associated with the risk of cognitive dysfunction"
Supplemental use of these vitamins has shown a slowing cognitive decline and also improvement in clinical status in patients with cognitive impairment, particularly in those with high baseline levels of serum Hcy [3]. A high circulating concentration of homocysteine has been implicated as a risk factor for Alzheimer's Disease and its prodromal stage, mild cognitive impairment. Cognitive and psychosocial impairment has been associated with increased levels of homocysteine [4]. While not a specific marker for schizophrenia, hyperhomocysteinemia occurred in our schizophrenia patients with poor social and relational functioning [5]. Elevations of serum homocysteine levels are a consistent finding in addictions. Hyperhomocysteinemia could enhance the substance consumption increasing the severity of craving in a circular self reinforcing mechanism. [6,7] MTHFR variants and smoking behaviour were associated with homocysteine plasma levels [8]
Folate deficiency is associated with depression, attention issues, and other neuropsychiatric disorders, along with irritability and behavioural problems. Cerebral folate deficiency has been linked to self-injurious behaviour. In ASD, "In clinic I have certainly seen some very beneficial effects of using the active forms of folate in ASD" [9] Inflammation induced by by low folate concentrations can significantly be attenuated through treatment with appropriate supplementation and result in cognitive function improvement and decrease of peripheral inflammatory cytokine levels
B12 deficiency has been "linked to agitation, irritability, negativism, confusion, disorientation, amnesia, impaired concentration and attention and insomnia; while psychiatric disorders that may be diagnosed in patients having vitamin B12 deficiency include depression, bipolar disorder, panic disorder, psychosis, phobias and dementia". B12 deficiency has presented in younger patients with “irritability, regressive behaviour, apathy, crying and truancy”
[1] https://news.osu.edu/hostility-anger-linked-to-chemical-that-may-cause-heart-disease/
[2] https://www.ncbi.nlm.nih.gov/pubmed/14724053.
[3] https://www.ncbi.nlm.nih.gov/pubmed/29936555
[4] https://www.ncbi.nlm.nih.gov/pubmed/29306698
[5] https://www.ncbi.nlm.nih.gov/pubmed/26017629
[6] https://www.ncbi.nlm.nih.gov/pubmed/28527647
[7] https://www.ncbi.nlm.nih.gov/pubmed/26885351
[8] https://www.ncbi.nlm.nih.gov/pubmed/23285280
[9] http://www.allnaturaladvantage.com.au/home/wp-content/uploads/2014/11/Cerebral-Folate-Deficiency.pdfAddressing serotonergic aspects
The emotional dysregulation was intense. It seemed to be hypothetically a very 5-HT deficient state
Both fear/terror and anger/rage are here further assumed to be low-serotonergic. Aggression has also been coupled to serotonergic deficit in many studies, supporting the placement of anger/rage on the low-serotonergic side
A first approach would involve the administration of tryptophan and/or BH4. Lack of tryptophan in the diet has been linked to decreases in tissue tryptophan and in brain serotonin - changes in tryptophan availability have a direct impact on the rate of 5-HT synthesis
Tryptophan enriched diets in animal models have led to increased prefrontal activation, these results seem to suggest that activation of the PFC could be related to a decrease in anxiety/diminishing amygdalar activity and to decrease in depression-related symptoms
L-tryptophan has shown efficacy as an isolated substance in the treatment of depressed patients (it lifted the mood of participants and affected the function of brain regions known to be associated with mood regulation), addition of tryptophan to fluoxetine was associated with a greater improvement within the first week of treatment. It also lessened the fluoxetine-induced decrements in slow wave sleep. There were no cases of serious toxicity of the combination; it was very well tolerated overall [1]. Serotonin syndrome resulting from augmentation of antidepressants with L-tryptophan is ‘rare’
It has found use in OCD as an augmentation strategy [2]
L-tryptophan was found to be a well tolerated and useful adjunct and standalone antidepressive agent in treatment-resistant unipolar depressed borderline personality disorder patients, with positive effects on sleep, suicidality and social engagement. [3]
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/11022398/
[2] https://www.ncbi.nlm.nih.gov/pubmed/9393391
[3] https://www.sciencedirect.com/science/article/pii/S221296261500036X
"Impulsive, violent and suicidal behaviours have repeatedly been shown to be associated with a reduction in serotonergic activity in the central nervous system. Tryptophan supplementation may be most effective in reducing aggression during times of stress.Tryptophan, an essential amino acid, is the dietary precursor to serotonin, and several lines of evidence have suggested that the amount of tryptophan in the diet relates closely to aggressive behavior. For example, rats given a diet almost lacking in tryptophan develop aggressive behavior
In a group of depressed alcoholics, those with a history of aggression, including suicide attempts, also had the lowest tryptophan ratios
When hospitalized male schizophrenics were given tryptophan, only those patients with high levels of hostility and a high lifetime frequency of aggressive incidents benefited; these patients showed a lessening of hostility and depression, a reduction in ward incidents and improvement on a standardized psychiatric rating scale."
Note: A diet high in Trp, but with a large amount of LNAAs (leucine, isoleucine, tyrosine, phenylalanine, and valine), will not result in higher brain Trp levels, and may even decrease Trp uptake into the brain. An intervention rich in Trp relative to other LNAAs (including is needed in order to boost uptake of Trp, and consequently serotonin production, in the brain.
It may be more difficult for the prefrontal cortex to control negative emotional responses that are generated within the amygdala under low serotonin, meaning Trp may help [1]
Low tryptophan levels may significantly affect the mood and may contribute to anti-social, aggressive and impulsive behaviours [2] Tryptophan metabolism is disturbed in abstinence
Experimental lowering of serotonin (5-HT) neurotransmission by acute tryptophan depletion (ATD) induces a transient depressed mood in 50–60% of patients treated with a selective serotonin reuptake inhibitor (SSRI) who are in remission from depression [3]. It has been claimed by some that simple dietary manipulation is not an effective method to increase brain Trp and 5-HT.
The effect of an SSRI on extracellular 5-HT are dependent on the nutritional availability of Trp. Moreover, increased availability of TRP affects behaviour in a manner similar to SSRI administration. While caution is advised, it's being explored as an augmentation strategy [4]
"...nutritional factors play an important role in the biosynthesis of 5-HT. Increasing 5-HT levels by increasing the availability of TRP might augment the therapeutic efficacy of SSRIs, whereas malnutrition may render patients refractory to SSRI treatment.”
Studies suggest long-term effects of dietary Trp on stress responsiveness
Acute tryptophan depletion caused a significant decrease in perceived control and increase in interfering thoughts at the time of provocation in OCD. "Successful selective serotonin reuptake inhibitor treatment of obsessive-compulsive disorder may involve the ability of serotonin to switch habitual responding to goal-directed behaviour." and it has been proposed tryptophan or 5-HTP may augment the effectiveness of antidepressants.
Trp supplementation seems to improve control over social behaviour in patients and individuals suffering from disorders or behaviours associated with dysfunctions in serotonergic functioning - in healthy humans supplementation seems to promote social behaviour [5].
Review: Effects of tryptophan loading on human cognition, mood, and sleep
[1] https://www.cam.ac.uk/research/news/serotonin-levels-affect-the-brain’s-response-to-anger
[2] https://www.salubrainous.com/tryptophan-for-alcoholism/
[3] https://www.sciencedirect.com/science/article/pii/S0165032705000182
[4] https://link.springer.com/article/10.1007/s00213-003-1632-6
[5] https://doi.org/10.1016/j.neubiorev.2016.02.022Part of the fun with effectively bolstering serotonergic activity is that positive beliefs come on line (or feel positively amendable), what were heavy cognitive self-referential processes taper down there's a socio-emotional dimension that comes on line and cognitive/behavioural flexibility bolsters.
Studies show that the relationship between the activation of serotonin and subsequent behaviour is highly dependent on the belief about the circumstances [1] Self-referential processing is a key cognitive process, associated with the serotonergic system and the default mode network (DMN).
"Typically, depressed individuals endorse more negative adjectives as self-referential than non-depressed individuals. This bias in self-referential processing is also present in individuals who have remitted depression, suggesting that negative cognitive biases persist even when symptoms are no longer evident."
"Analytical self-focused rumination (thinking analytically about self and symptoms) is maladaptive - This cognitive style is associated with overgeneral autobiographical memory, global negative self-judgments, greater negative future thinking, and dysphoria." It appears to reflect DMN connectivity which can be modulated by TRP [3]
[1] https://www.eurekalert.org/pub_releases/2018-06/oios-wfi053018.php
[2] https://www.sciencedirect.com/science/article/pii/S016801021002835XThere are a few 'side effects' to Trp
While "involvement of 5-HT in rewarding and aversive processing, hedonic experience, mood and higher cognitive functions such as consciousness or self reflection are undisputed" and there seems to be a good level of "contentedness" and mood/emotional regulation...
Manipulations of serotonergic tone affect reward [1] and decision making [2]. Depleted states cause one to be significantly more perseverative over choices and acutely significantly less sensitive to reward (lower reward magnitude)
For me, the impulsive reward chasing loops start to seemingly undergo some changes (serotonin has been proposed as a possible encoder of reward and facilitator of reward extinction): you go from impulsive action to greater conscious choice but it doesn't feel as rewarding to do things. It's a little blunting. So those healthy addictions, for me gardening and daily walking, start to feel more effort-driven than impulse driven and require more effort in. If you're not careful, you can become content with inaction.
Depletion of 5-HT enhances behavioural and brain responsiveness to aversive signals, while disinhibiting previously rewarded but now aversive behaviours. [3]
You start to seemingly have a layer of higher order self-reflection come in. You want better choices. It has been proposed "5-HT encodes beneficialness, and may signal motivation to either maintain or switch current behaviour, for example displayed by 5-HT’s role in facilitating patience for future rewards"
[1] https://www.frontiersin.org/articles/10.3389/fnhum.2017.00484/full
[2] http://www.jneurosci.org/content/32/17/5833
[3] https://www.ncbi.nlm.nih.gov/pubmed/18069045-
 4
4
-
-
Do any of the nornicotine dominant Nicotiana have a history of traditional interesting use?I'm trying to suss out the novel tobacco's. I'm sick of relapsing on boring NRT nicotine only.From what I can find, N. tabacum, N, rustica, N. alata, N. langsdorffii all contain nicotine; N. sylvestris and N. rusbyi [N. tomentosiformis] contain nornicotine, while N. glauca contains anabasine.I've used N. glauca cautiously but didn't get heavily into it [covered the potential anti-addictive nature of anabasine in [1]] and the major nicotine containing Nicotianas. I want something different. I want to know what nornicotine is like as a dominant alkaloid? Exploring some cotinine would be neat, the predominate metabolite of nicotine, which has been "shown to reduce depression, anxiety, and fear-related behaviour as well as memory impairment in animal models of depression, PTSD, and Alzheimer's disease." [2]."Nornicotine (N-desmethyl-nicotine) appears to activate different nAChR subtypes, has a better pharmacokinetic profile, and produces less toxicity than nicotine." [3]Note: the nornicotine in Duboisia hopwoodii has been stated in one (albeit old) paper to be d-nornicotine contrary to what is found in Nicotiana, which may be more toxic, potentially giving rise to the statement "Twentieth century chemical analysis found that both nicotine and nornicotine, a drug four times as toxic as nicotine, are usually present in Duboisia" [4].Nornicotine occurs in several species, such as Nicotiana sylvestris and some Australian species [5].N. sylvestris contained 0.44% alkaloids in one study but in another, had a total alkaloid concentration of 1%, nornicotinecomprising 95% of the alkaloids [6]. Another reference [8] gives 4.8mg/g alkaloids, 82.2 % of that being nicotine.Nicotiana langsdorffii contained 0.22% alkaloids, 73% being nicotine, the rest nornicotine [7].It is the dominant alkaloid in N. thyrsiflora (94.3% of the 5.1mg/g total alkaloids). It is said "The heated leaves of Nicotiana thrysiflora are used for rheumatism." In Nicotiana tomentosiformis, nornicotine makes up 79% of the 1.1mg/g total alkaloids. N. glutinosa contains 7.4mg/g with 77.4% of that being nornicotine [8]."About 0.8% of nicotine is metabolized to nornicotine in the periphery. However, the biotransformation of nicotine to nornicotine also appears to occur locally in the brain, and brain concentrations of nornicotine have been shown to exceed those in the periphery" [9].Nornicotine is proposed to result in additional activation of a7-type receptors, which may be important for effects on cognition and attention. Nornicotine inhibits striatal DAT function via a nAChR-mediated mechanism [10]. "The nAChRs mediating the nornicotine-induced inhibition of DAT function appear to be different from those activated by nicotine which increases DA clearance"Both nicotine and nornicotine were relatively potent partial agonists of rat α7 receptors with efficacies of approximately 60% and 50%, respectively, compared with AChThe efficacies of nicotine and nornicotine for α4β2 receptors were relatively low, compared with ACh, although nicotine was rather more potent than nornicotine and ACh. Nicotine was relatively efficacious for α3β4 receptors, although less potent at α4β2 receptors. Nornicotine was a relatively poor agonist for α4β2 and α3β4 receptors.The half-life of nornicotine in brain is 166 min, which is three times longer than that of nicotine (52 min)For more nicotine containing plants:For a breakdown of normal tobacco:Alkaloids 11.462 mg/gNicotine 94.8%Nornicotine 3.0%Anabasine 0.3%Anatabine 1.9%N. alata is generally very low on nicotine but allows the other non-alkaloid constituents of tobacco's medicine to be explored.N. megalosiphon contained 0.22% alkaloids, 100% being nicotineN. quadrivalvis had in one study a nicotine content of approximately 0.16% in one study. It was the main native tobacco that was once widely cultivated by numerous tribes for medicinal and religious purposesAnother reference givesAlkaloids 7.76 mg/gNicotine 94%One early trier found the such tobacco "very pleasant," adding, "it does not affect the nerves in the same manner..."Alkaloids 8.945 mg/gNicotine 98.5%Nornicotine 0.3%Anatabine 1.2%
Thanks @Micromegas
-
Background: Elixirs conferring eternal youth or inducing amatory and erotic attraction have been searched for without success. Lovesickness is a widespread affliction resulting from unrequited love and/or the impossibility for physical and emotional union. The symptoms are reflections of altered dopamine, serotonin, noradrenaline, testosterone and cortisol levels and range from frenzy and intrusive thinking to despair and depression, sharing traits with the neurochemistry of addiction and compulsive behavior disorder. Although it can seriously impact the quality of life, lovesickness is currently not considered in official disease classification systems. Consequently, no official therapeutic guidelines exist, leaving subjects to seek the cure on their own.
Methods: We review literature of the past 2000 years dealing with the concept, diagnosis and the healing of lovesickness and contextualize it with neurochemical, ethnomedical, and ethnographic data. Since neurobiological and pharmacological connections between the love drive and the sex drive exist, we review also the literature about herbal an- and aphrodisiacs, focusing on their excitatory or calmative potential.
Results: An overall consensus regarding socio-behavioral regimes exists for dealing with lovesickness from historical through contemporary literature. The herbal drugs used for treating lovesickness or inducing love passion do not possess the alleged properties. The pharmacological effects of aphrodisiacs are heterogeneous, including dopaminergic and adrenergic activities, but there is no evidence for any serotonergic effects. The libido-regulating properties of anaphrodisiacs seem to be associated with sedative and toxic effects or decreasing testosterone levels. CB2 receptors expressed on dopaminergic neurons of the ventral tegmental area, part of the brain’s reward circuit, implicated with addiction, orgasm and strong emotions such as love, might constitute a new therapeutic target.
Conclusion: The common food additive and CB2 agonist β-caryophyllene might have the potential to attenuate dopaminergic firing, quenching the reward and thus motivation associated with romantic love. From Greek mythology to modern history, cultural expressions and implications of love, sex and procreation is and was organized along hierarchical lines that put men on top. The neuronal predispositions and activities associated with falling in love will probably forever remain nature’s and Eros’ secret.
Copaiba oil, ~50% β-caryophyllene, appears safe orally at low doses
An update on the pharmacology of BCP
- orally active potent CB2 full agonist and PPARα/γ agonist.
- Analgesic, anti-inflammatory, anti-amyloidogenic, insulin-sensitising, anti-alcoholism, anti-cancer, cardioprotective, hepatoprotective, gastroprotective, neuroprotective, nephroprotective, antioxidant, antimicrobial and immune-modulator effects
- Exerts anxiolytic and the anti-depressant effects via CB2 agonism
- Activates TrkA receptors and induces neuritogenesis by a mechanism independent of NGF or cannabinoid receptors
- potent antagonist of α7-nAChRs
- exhibits synergy with µ-opioid receptor dependent pathways
- Neuroprotection via prevention of microglial activation and inflammatory cytokine and chemokine expression: β-caryophyllene reduced astrogliosis and microglial activation as well as the levels of COX-2 protein and the mRNA levels of the proinflammatory cytokines tumor necrosis factor-α and interleukin-1β in the cerebral cortex, inhibits pathways triggered by the activation of toll like receptor complex
- CB2Rs modulate striatal dopamine release
- PPARγ activation prevents the negative emotional effects of stress and exerts anxiolytic actions
- CB2 agonists may provide therapeutic possibilities to treat metabolic diseases associated with lipid dysregulation.β-caryophyllene is an attractive molecule with therapeutic potential for the treatment of pain, Alzheimer's disease, anxiety, depression, Parkinson's, schizophrenia, various neurodegenerative conditions, brain injury, diabetes and metabolic disorders
-
 2
2
-
-
Yeah, feel you on that, sorry to hear things are a struggle for you. I got disconnected again and the only way I've recently been able to reconnect is through plants. It takes my head off the social situation which is hard to manage with anxiety, social anhedonia and not finding common ground etc.
Churned out a bunch of Ashwagandha tubestocks through winter that did well in the greenhouse, ready for spring. Joined the local grow free group. I've been forcing myself to connect with new people, even strangers, by giving the plants away. It just makes an awkward social encounter more positive. A reason to try.
Just breaking that pattern of isolation through a plant can be potent. You can rebuild some social skills etc. Transfer interests from one domain to another etc-
 2
2
-
-
Tomorrow, spike those ketones in the name of a healthy brain experiment and see what I think of it as a "neurotherapeutic" and "promising anxiolytic strategy" [1], see if there are hints of enjoyable prosociality which would be nice. "Use of βHB as an efficient neurotherapeutic relies on increasing blood βHB levels so as to encourage entry of βHB to the brain." [2]
The main problem with using βHB as a therapeutic lies in being able to deliver sufficient βHB to the brain, due to the limited uptake of βHB across the blood brain barrier and the difficulty in sustaining high enough levels of βHB in the blood - uptake can be increased by instigation of dietary changes, such as a high fat diet or regular ingestion of medium chain fatty acids.
Any keto nuts suggest better (other than ketone esters) than BHB+MCTs? I want to feel it as acutely as possible... Thinking to go from intermittent fasting/low carb to using short term BHB + MCTs as my diet for a bit.
Ketone bodies upregulate neurotrophins, reduce neuroinflammation and hyperexcitability, causing potent neuroprotection. They also drive growth and myelination, enhance synaptic plasticity, cognition and neuronal stress resistance, improving learning and memory. Exogenous ketones also improve oxygen utilisation, especially in the central nervous system
There are concerns regarding the level of Ca and K provided by supplementing BHB salts, which can rise to toxic levels if excessive doses are administered, so adherence to dose recommendations is required [3]
In the body, "Exogenous ketone supplementation causes blood glucose to decrease significantly, likely due to the acute increase in insulin sensitivity. Therefore, exogenous ketones may present a potential therapy for type-2 diabetics via regulation of blood glucose.".
"BHB + MCT raises blood BHB levels much higher than BHB or MCT in isolation, with a peak just over 1.30mmol/L. Even more important is that blood BHB levels do not seem to readily fall back to the normal levels of 0.2mmol/L. Even after 8 hours blood BHB levels are 0.5mmol/L, which is over double the normal level, and they look to be only very gradually falling. Blood BHB levels look like they will be elevated for the best part of a day, but the most significant rise being between 1 and 4 hours after ingestion." [4]
Consumption of MCTs produces a mild ketosis which has been estimated to contribute up to 8–9% to brain energy metabolism and it is well tolerated.
In comparison, "In human tests, 30ml of MCT oil was able to raise blood BHB levels to about 0.55 mmol/L. This is just over half the effect that BHB salt supplementation had. MCT oil supplementation spiked blood BHB levels at just under an hour, and drops to normal levels after 3 hours. Interestingly, BHB levels continue to fall below normal levels of 0.20mmol/L to 0.12mmol/L. The low blood BHB levels show no real indication of normalising after 8 hours."
While the low ketone levels generated by MCT supplementation have been demonstrated to partially reverse the memory deficits of Alzheimer’s dementia, exogenous ketones have the potential for greater memory-improving effects, with maximum effect likely occurring at a beta-hydroxybutyrate blood level of 4 mmol/L or higher, the level at which ketone transport into the brain is maximised.
Human pilot studies and case studies suggest that ketogenic diet and ketogenic supplement-induced ketosis is a potential therapeutic approach in the treatment of epilepsy, Alzheimer's disease, autism spectrum disorder, and schizophrenia
Ketone bodies may exert their effects through modulation of GABAergic, glutamatergic, and adenosinergic system. Administration with no need for energy restriction might also be a promising intervention to improve the neuronal activity and ameliorate the degeneration of CNS.Noted antidepressive and anxiolytic effects
It an efficient mitochondrial fuel, improving energy metabolism
Enhances GABAA receptor function, upregulates GABAergic activity [may increase GABA concentration], enhances inhibitory glycine receptors
Decreases brain glutamate, alters the response of NMDA receptors, L-type Ca2+ channels, reduces neuronal firing rates, mediated in part by Katp channel activity and GABAB signaling
It interacts with an inflammasome in immune cells to reduce production of inflammatory cytokines and reduce inflammation.
inhibitor of histone deacetylases resulting in upregulation of genes involved in protection against oxidative
stress and regulation of metabolism
Supplementation with βHB has been shown to extend the lifespan of C. elegans by 20%[1] https://www.frontiersin.org/articles/…/fnmol.2016.00137/full
[2] https://www.ncbi.nlm.nih.gov/pubmed/27826689
[3] https://blog.undoctored.com/beware-exogenous-ketones/
[4] https://ketosource.co.uk/exogenous-ketones-how-they-work/By afternoon, I'm normally crashing in mood, grumpy and tired, not that the morning is much better. I got a paradoxical lift changing my diet for once, but then the typical diet shift anergia kicked in.
From a couple of days of IF, gave the BHB salts a whirl. Solid dose, 12g BHB and some MCTs. Really, the ketone elevations offered by even large doses of the salts aren't that huge but "can help your body transition into ketosis with less misery and hunger pangs." potentially. The combo of MCTs and BHB is said to be better for BHB elevations.
Beta hydroxybutyric acid is antidepressive and anxiolytic. It enhances inhibitory glycine receptors at concentrations observed in humans clinically. In addition, beta-hydroxybutyric acid enhances GABAA receptor function at these concentrations. Subanesthetic concentrations may contribute to lethargy and impairment of consciousness [1] and has abilities to alter physical properties of cell membranes [2]
[1] https://www.ncbi.nlm.nih.gov/pubmed/17717222
[2] https://www.ncbi.nlm.nih.gov/pubmed/23339286By 45min, there's a very mild energetic lift, wouldn't say much more than MCTs alone. Some restoring energy, stability of mood again and a little potential anxiolysis. Functionally nice as a mild meal tonic. Enough to get another bout of exercise in, which seemed to attune me to it more.
It was pleasant exercise. Just a calm, centred functional bit of exercise. Didn't feel so neurotic.
Got for another bit of exercise - just level headed.All in all, maybe the BHB salts are useful but not likely to be problematic.
It may be therapeutically useful to for the times I crave alcohol (I've now been abstinent quite awhile),
"In ethanol dependence, it is suggested the following occurs "energy deficiency (“starvation”) of the brain → stimulation of production of ketone bodies → partial transition of the brain from exclusive using of glucose as the energy substrate to partial use of ketone bodies as such substrate. Under such conditions, the brain begins to be dependent, to a significant extent, on the level of these bodies in the blood, i.e., on the degree of ketonemia. With any decrease in this index, the biological requirement to replenish the amount of these compounds develops. Since rapid synthesis of ketone bodies can be readily initiated by introduction of ethanol into the organism, this organism tries to realize the corresponding behavioral reaction, i.e., to consume alcohol." [1]
MCTs themselves compensate for the brain energy deficits in direct proportion to the level of plasma ketones achieved. MCT-fed rats exhibited reduced anxiety-like behaviors and enhanced social behaviour [2] Data on the neuroprotective capacity of MCT-derived medium chain fatty acids (MCFA) suggest 8-carbon and 10-carbon MCFA may have cognition-enhancing properties which are not related to ketone production [3]
[1] https://link.springer.com/article/10.1007/s11062-016-9596-4
[2] https://www.ncbi.nlm.nih.gov/pubmed/29908242
[3] https://www.ncbi.nlm.nih.gov/pubmed/27517611-
 1
1
-
-
Recently got into the fasting. I like the mood stability and uplift.
Firstly has anyone used the commercial 'BHB exogenous ketone' salts and got an acute nice noteworthy mood reaction? There are commercial βHB salt products - quite pricey - but I want to know if anyone has heard of the cheap ketone esters, particularly super cheap (and fragrant!) ethyl acetoacetate, being used safely orally?I'm not going to slack off using will power to fast for my added uplift but I'm curious... it could be quite nice as an acute quite enjoyable mood lifter. Is it the βHB, or is acetoacetate a nice mood lifter? Ketones, particularly BHB, upregulate GABAergic tone but are they 'enjoyable' acutely orally administered?
"...researchers don’t know the exact cause of these [euphoric] feelings. Acetoacetate, acetone and BHB, or any of their metabolites, may all be involved, as well as the effects of low blood sugar, which can cause euphoria and giddiness."
People felt remarkably well, and experienced a mild intoxication:
not dissimilar to the effects of ethanol.Bloom speculated that acetoacetate had caused the inexplicable jubilation. [1]
Aside from acute prosocial anxiolytic effects which I deem as an important therapeutic area to address in many conditions, I'm also primarily looking for sustainable better health in my life, as are many people with epilepsy, Alzheimer's disease, autism spectrum disorder, and schizophrenia etc. My intermittent fasting is proving interesting, mood stabilising and uplifting in conjunction with other measures, pushed that quite a bit but it's personally not sustainable to run an extreme 'deprivation diet'. Just skipping breakfast and healthy meals at the other times with my exercise is probably my best bet. There are a few suggestions on ways to stay in a fasting state during IF [1].
Caved in and thought I had to try the most economical βHB salts, to get a gauge on it's effects. Probably get around to doing some trials with that this week. It is suggested elevations of β-hydroxybutyrate may partly mediate the beneficial effect of IF in CNS conditions. "Brain BHB concentration increased from a nonfasted level of 0.05 +/- 0.05 to 0.60 +/- 0.26 mM (after second day of fasting), increasing further to 0.98 +/- 0.16 mM (after the third day of fasting)" [2]
While βHB salts or other supplements "aren’t a great fat loss tool – they’re simply ways of increasing your blood ketones" and increase energy in, I'm more generally looking for the therapeutic benefits of ketones on the brain for the moment. Both would be nice - I'm getting really good kJ intake reductions and maintaining my exercise so hoping.
Unfortunately, with exogenous ketone administration, blood βHB reached low levels (<1 mM) and a high amount of salts, consumed βHB, was required to achieve ketosis. That said, this is still roughly equivalent to three days of fasting. That said, gastrointestinal symptoms were reported in a large number of participants. βHB has antidepressant and antianxiety-like effects and results in modulation of multiple systems, including GABA, Glu, adenosine, neurotrophic etc and even in the presence of glucose exerts beneficial CNS effects, also exerting epigenetic effects (β-hydroxybutyrate is a HDAC inhibitor).
Dietary ketone salts are often racemic mixtures of the two optical isoforms of βHB, despite the metabolism and actions of L-βHB being poorly understood
~12 or ~24 g orally administered ketone salts elevated D-βHB concentrations (D-βHB Cmax 1.0 mM) which returned to baseline within 3–4 h. [3] [Another study found 0.5 g/kg bw at 2 h elevated D-βHB, with a mean value of 0.598 ± 0.300 mM [4], 0.38 g/kg bw caused only a rise to 0.3-0.4 mM βHB in trained athletes [5]. The ketone salts contain 50% of the L-βHB isoform, which remained elevated in blood for over 8 h. L-βHB is still neuroprotective but not much is known about it's CNS effects
More cheaply, one can increase βHB in the brain 90 minutes after ingesting coconut/MCT oil, which improved paragraph recall in adults with impaired memory. Preliminary studies also show ketones can improve working memory in both young and old subjects
[1] http://siimland.com/what-breaks-a-fast-while-intermittent-fasting/
[2] https://www.ncbi.nlm.nih.gov/pubmed/11043913
[3] https://dx.doi.org/10.3389%2Ffphys.2017.00848
[4] https://www.ncbi.nlm.nih.gov/pubmed/29850235
[5] https://www.ncbi.nlm.nih.gov/pubmed/29966721"Conversion of ketone bodies (KBs) to ketone esters (KEs) eliminates KB acidity, making the KEs suitable vehicles for the delivery of KBs to the blood circulation via the gastrointestinal route. Ingestion of KE can directly increase plasma KBs to levels within the range achieved during fasting. The degree of KB elevation attained is readily controlled by the dose size
Studies have demonstrated that orally or intravenously administered 1,3-butanediol or glycerol esters of βHB are safe and well tolerated in animals and that the orally administered 1,3-butanediol monoester is also safe and well tolerated in humans" [2]
While 1,3-butanediol esters are ideal as they are readily metabolised in a manner similar to ethanol without the deleterious effect of ethanol metabolism, with subsequent conversion to βHB and, eventually (at the peripheral tissue level), to AcAc, I'm curious if ethyl acetoacetate might be healingly enjoyable orally administered?
While using diet is superior for weight loss than supplementation, there are a few people talking of acute βHB effects @12g of the salts: "...there was an unmistakable uplift in mental clarity, mood and energy. This continued for a number of hours. The energy & focus was clean"
It seems βHB is nicely anxiolytic in studies but maybe not intoxicating, the anxiolysis correlated with increased level of βHB .
Human pilot studies and case studies suggest that ketogenic diet and ketogenic supplement-induced ketosis is a potential therapeutic approach in the treatment of epilepsy, Alzheimer's disease, autism spectrum disorder, and schizophrenia.
Ketone bodies may exert their effects through modulation of GABAergic, glutamatergic, and adenosinergic system
It has also been demonstrated that administration of exogenous ketone supplements (normal food + ketone supplements and/or medium chain triglyceride/MCT), such as ketone ester (KE), ketone salt (KS) or their combination with MCT oil (e.g., KSMCT) induce rapid and sustained nutritional ketosis
https://www.frontiersin.org/.../10.../fnbeh.2018.00029/full
"Administration with no need for energy restriction might also be a promising intervention to improve the neuronal activity and ameliorate the degeneration of CNS" [6]
Just curious, couldn't spot it done anywhere...
From risk assessment of Ethyl Acetoacetate
Acetoacetate is an endogenous product of accelerated fat metabolism.
Absorption of ethyl acetoacetate via the oral route is demonstrated in animals
It may be anticipated that ethyl acetoacetate is partially cleaved already in the gastrointestinal tract due to acidic pH values or by bacterial activity. In a first metabolic step the absorbed portion of ethyl acetoacetate will be hydrolysed into 3-oxobutanoic acid and ethanol by the unspecific esterases of the blood. The acid moiety is an endogenous product within the lipid metabolism and is further metabolized predominantly to carbon dioxide and water; ethanol will be metabolized on known pathways.
In animals, acute toxicity by the oral, dermal, and inhalative routes is low as judged by tests with rats. The substance demonstrated no or only mild skin irritation and mild eye irritation in tests with rabbits. Valid human or animal data on sensitization are not available.
Following repeated oral exposure of ethyl acetoacetate in rats, no treatment-related adverse effects (including haematology, clinical chemistry, gross necropsy and histopathology) were reported up to 1,000 mg/kg bw/d.
Note: Levels above 10 mmol/L of ketone bodies are associated with ketoacidosis.
-
Thanks for the kind words @Xperiment Likewise, had been wondering how you were traveling. Hope things are OK, feel free to chat with a message if ever needed. It's nice to not be in the continued pep of mixed weird moods, which turned into a bit of a nose dive, driven by grief and anger and other emotions I was struggling with in part but it's nice to get a day like today where I had the balance of positive mood, social contact, meaningful activity all working etc.
-
I needed a bit of extra help with my mood over winter so went back on a minimal SSRI dose. Recently, I've been cautiously exploring how things like turmeric and saffron to go with that SSRI, which I don't find alone effective. The spices etc seem quite tailorable to be used to 'level up' when mood needs a more acute lift.
. I've explored conventional pharmacotherapy extensively, shifting thinking/psychological stuff and other strategies, with little sustained benefits, at many times the side-effects of conventional pharmacotherapy caused more problems than solutions and sent me off dangerously self-medicating. Also I've explored herbal options too, finding some that some helped somewhat with excellent side-effect profiles.
I'm currently giving the synergy of healthy dietary phytochemicals and minimal Western medicine a go. Does it hold promise, the best of both worlds for treatment resistant conditions? I still side with improvements being bio-psychosocial-spiritual but if you're biologically bed-ridden/housebound with debilitating symptoms, you can't tackle the other dimensions properly.
One thing I'll say, is conventional pharmacotherapy as a standalone for mental illness is poorly effective for MANY people. Even coupled with psychological stuff. That said, our plant medicines aren't panaceas. Diet doesn't cure everything.
The medicinal spices had enough potential merit, tolerability, evidence-base and safety to make it something worth considering as continued tools, especially useful for milder symptoms but efficacy waned relying on it as standalone for myself, as things like my fermented turmeric concoctions. While curcumin alone shows antidepressant efficacy, supplementary administration of curcumin to antidepressant therapy may reverse the development of depression and enhance the outcome of antidepressant treatment, also offering more rapid relief of depressive symptoms [1]. Same with saffron, it's got me through some really dark times off antidepressants but once again, efficacy waned for mood. Saffron did seem unique for psychotic spectrum stuff, crocins not only modulate the HPA axis and NMDARs but the DAergic system in a way that may be of relevance for schizophrenia-like behavioural deficits. These spices are useful tools and seem to have limited potential for interactions with SSRIs. While saffron is useful alone, showing efficacy equal to SSRIs [2], saffron could effectively prevent reaching the criteria of metabolic syndrome [3] and it significantly augmented SSRIs, both reducing side effects [4,5] and augmenting efficacy [6]
I normally use bulk Iranian saffron but spotted a cheap Saffron + Curcumin (BCM-95, which is turmeric volatiles enhancing the bioavailability of curcumin, so piperine interactions with pharmaceuticals aren't problematic). I found I could kind of chase a saffron buzz a bit, as this product, I might be more sparing.
[1] https://www.ncbi.nlm.nih.gov/pubmed/26066335
[2] https://www.ncbi.nlm.nih.gov/pubmed/27701683
[3] https://www.ncbi.nlm.nih.gov/pubmed/24955550
[4,5] https://www.ncbi.nlm.nih.gov/pubmed/23280545 https://www.ncbi.nlm.nih.gov/pubmed/22552758
[6] https://www.ncbi.nlm.nih.gov/pubmed/25484177My mood has been so pathological, absolutely crap, so I'm trying a few things at once. Got into waking early (partial sleep deprivation as needed), keeping up exercise and skipping breakfast and having ALCAR as a meal replacement.
have to tackle my body and brain at the same time particularly before they get even more out of whack, the two are linked. Things like saffron are established as being useful preventing metabolic abnormalities but ALCAR is cheap.
"Scientists have noted a connection between depressive disorders, primarily seen as brain-based, and, insulin resistance (IR), a modifiable metabolic pro-inflammatory state that is typically seen as peripheral. Treating IR can with drugs or behavioural interventions can ameliorate, or possibly prevent, depressive disorder and its long-term consequences including dementia at various stages of the life course.
Acetyl-L-Carnitine (LAC) is an endogenous molecule that regulates glutamate homeostasis and promotes healthy mitochondrial function, among other actions.
Acetyl-L-carnitine presents a significant link between altered peripheral and neural function in the context of stress and depression.
It has epigenetic action in reactivating neuroplasticity by restoring an inhibitory tone upon the release of glutamate driven by elevation of a stress-induced decrease in histone acetylation.
Administration is also known to ameliorate insulin sensitivity in patients with type 2 diabetes
Disruption of LAC function is an example of a molecular mediator that indicates a lack of resilience leading to negative outcomes. Indeed, epigenetic alteration of LAC is a marker of IR. Importantly, modulation of LAC levels is an example of capacity for flexible adaptation—thus LAC function can be reinstated and result in amelioration of changes associated with glutamatergic damage.
LAC supplementation while targeting IR (i.e., reducing peripheral hyperglycemia, hyperinsulinemia, and hypertriglyceridemia) leads to antidepressant-like responses seen after few days of administration, while responses to standard antidepressant medications require repeated weeks of administration in the same animal models"
https://www.ncbi.nlm.nih.gov/pubmed/29180223
Full text: http://sci-hub.tw/10.1016/j.neuropharm.2017.11.038
Quickly, that combination resulted in a good mood improvement and symptom reduction.
-
 1
1
-
-
I can do you a turmeric and a un-ID'd galangal if you cover postage? Also Alpinia zerumbet. They're all shoots off the main plant.
A. zerumbet is truly a multi-purpose ginger plant with promising medicinal properties." [1]
"Shell ginger is an exceptional multi-targeted plant for human use, considering various organs, diseases, and mechanistic actions. As it presently stands, the plant’s potential for human life is likely underestimated." Apparently, Alpinia zerumbet has leaves that make a tasty tea. I've tasted a little bit of rhizome, got quite a refreshing taste, the tea from the leaves is personally quite mild in flavour but pleasant.
Leaf extracts of A. zerumbet and A. zerumbet ‘Variegata’ ranked first and second among five Alpinia species screened for phenolic contents and antioxidant activities
There was some interest on kava forums with regard to it, even though the kavalactones might not be the more renowned 'euphoric' ones.
Alpinia zerumbet has anti-hypertensive, anti-obesity, anti-diabetic and sedative etc properties. The major bioactive phytochemicals are dihydro-5,6-dehydrokawain 0.41% in leaves and 0.35% in rhizomes and 5,6-dehydrokawain [Desmethoxyyangonin], and essential oils, phenols, phenolic acids, and fatty acids. Kava is able to increase dopamine levels in the nucleus accumbens and desmethoxyyangonin likely contributes to this effect. Literature now suggest that culinary shell ginger may contribute to longevity [2] The kavalactones are found in fresh leaves, stems and rhizomes range from the highest amounts of dihydro-5,6-dehydrokawain per fresh weight were detected in leaves, followed by rhizomes, and stems, whereas the reversed constellation was found for 5,6-dehydrokawain with the highest contents in rhizomes and lowest ones in leaves.
Leaves, at higher doses, exert antidepressant effects through the dopaminergic and/or noradrenergic system, with antioxidant and anxiolytic-like effects [3]. It also contains labdane-type diterpenes and leaves contained considerable amounts of total polyphenols. The 'Variegata' is an aromatic medicinal plant, its foliage producing an intense, unique fragrant odour due to 1,8-cineole, p-cymene, humulene, camphor, linalool, (E)-methyl cinnamate, gamma-cadinene, humulene oxide II and a-terpineol.
[1] https://www.researchgate.net/…/321396609_Alpinia_zerumbet_a…
[2] https://www.ncbi.nlm.nih.gov/pubmed/29385084
[3] https://www.ncbi.nlm.nih.gov/pubmed/25885936-
 2
2
-
-
-
On 4/23/2017 at 3:27 PM, TommyChesnutt said:Salvia Guaranitica is certainly active. Contains Cirsiliol, comparable to ambien. Works noticeably well. Only other species you'll find with any noticeable psychoactivity, imho.
What doses of Salvia guarantitica are people finding active?
Even though my interest in sedative plants has declined recently, on the contrary I now need pep...

There were questions as to how effective Salvia guaranitica would be:
.
That said, I want to find exactly what the "high concentrations" of cirsiliol are in the plant, I can't spot anything? It may be feasible to get 2mg/kg (active i.p dose in mice), which is quite low in human equivalence - that said, It does seem odd to me that a flavonoid is reasonably potent with it's low affinity?
Salvia guaranitica is used as a traditional medicinal plant used in Latin America as sedative. Studies demonstrated the presence of cirsiliol in its extracts and found that this flavonoid is a competitive low affinity benzodiazepine receptor ligand. Sedative and hypnotic properties of the ethanolic extracts of S. guaranitica (Medina et al., 1989) have been associated with the presence of high concentrations of the flavonoid cirsiliol and caffeic acid ethyl ester (Mader et al., 1996). Cirsiliol 2 mg/Kg, i. p. significantly decreased the number of head dips and rearings in the holeboard test, which indicates sedative action (Wolfman et aI., 1994). Moreover, cirsiliol at a dose of 4 mg/Kg, i. p., exerted hypnotic effects [1] Salvia guaranitica extracts and its active principle cirsiliol, possess sedative and hypnotic properties at a dose equivalent to 3g of the fresh leaf; cirsiliol produces these effects probably acting on the benzodiazepine receptor. [2] It also contains caffeic acid ethyl ester, also with affinity for GABAARs. The paper states: "additional active principles present in Salvia guaranitica and possessing synergistic action with cirsiliol can not be totally ruled out"
Saw a great initiative from beyondblue - they've released a Salvia guaranitica - 'Black and Bloom'. Not only do you get a pretty plant but a traditional medicine plant. As I'm finding, these plants are tough as seem to thrive. Proceeds from the sale of Black and Bloom go to the beyondblue foundation. Hopefully more plant retailers start to sell these, first time I've spotted them.
With a hardly responsive GABAergic system and having a baseline of a really low mood, they seem mild.
Plants are relatively small but some oral experiments, in conjunction with some healthy dietary modification:
"Amistad": At 4g fresh younger leaf, easily a placebo, nothing really noted other than possible very mild relaxation
"Black and Bloom" At 4g fresh mature large leaf, it seemed very mildly calming, easily placebo. At 8g still relatively mild, easily placebo.
"Black Cobalt" mature large leaves, jumped in at 10g and this one seemed possibly more active but it was more likely I was having a slightly better day @ 7g spent morning in the garden and felt OK, easily placebo
-
 3
3
-
-
I've been continuing this quite awhile hoping it would make a standalone anti-depressant option for me. The seasonal shift has been intense for me. If anything, it's brought some stability but actually confronted me with new levels of existential distress
That classic K10 question "how often did you feel worthless" so pressing... this scary crushing sense of my mortality imbuing this impetus to do things worthwhile and positive even when things are a struggle. Normally, I'd be in quite a suicidal state, where you're actually encouraging that process of death to hurry up but when you start seeing the bigger picture, in a more clear-headed and less pathological state of mind...
Coming out of that seemingly super-inflammatory state - I strongly believe inflammatory mediators, as research suggests, strongly promote a general trade-off towards focusing on immediate (often maladaptive) versus delayed (often more eudaimonic) outcomes while leading from everything to mood issues, anger problems to impulsivity - has been strange, not being pepped pathologically, forcing me to be reconsidering what the hell I'm doing with life. It's not easy finding that meaning, purpose and contribution when you're not feeling the greatest but I'm trying to make small positive vibrational shifts.
Probiotic turmerics, even with saffron, is not providing good stable uplift - Been sticking with it, hoping the mood support would be adequate.. It's easing some symptoms but the mood has been incredibly 'sanely depressing'. Been trying to give the anhedonic, anergic, apathetic moods a kick in the arse by keeping up exercise (it's reduced in vigour as I'm just so drained), gardening and exerting meaning and purpose but it's not working very well.Been chipping away at incremental meaningful stuff but plagued by quite an intense and anergic dysphoria, at best anhedonia - what I was trying to keep on top of and had slight success for a bit... Been painfully fighting the inner death drive with lots of potting up plants for others and propagating things that will hopefully cope with the weather, sounds small but all I can manage. The "life output" trays are filling up again, trying to give the barrage of morbid looping thoughts the finger but it's a battle.
Trying to assert some simple meaning and break my mind from the loops of depressogenic thoughts, maintain some behavioural activation even though it's so energetically hard, haven't had a energetic shift like this in a long time. Been a long time without my serotonin transporters occupied and continual serotonergics... finding aiming for the social can amplify things the wrong way at the moment, yet trying to not get extra disconnected.
-
 1
1
-
-
Yeah I sort of came to the conclusion it probably needs longer term dosing over acute. At 3g I got mild effects improved sleep quality (with atypical vivid dreams) but I'm not the best test subject. I don't know how stable the galphimines are thermally but I probably wouldn't smoke, if anything "The plant’s dried leaves and flowers are macerated in alcohol and shaken by hand to obtain the required potency." [1]
That said, I had someone with diagnosed GAD try it and they found it gave them an early sleep and said "Definitely find it calming". Maybe if there's nothing too pathological, like hyper-excitability etc, it's not too effective? -
I'll sort out the above. No problems @mole. OK we'll leave it there. If anyone gets desperate for some seed, let me know, otherwise it's available other places, let me know if you can't find others.
-
Can spare a few people some free seed [and/or smallish quantities of research material (in exchange for an opinion in a thread)].
I'll say the first three people? Can probably do more if someone's really keen, just keeping some seed for plant meets etc.
Post here then shoot me a PM."Best time to sow is late autumn and winter in good quality seed raising mix, cover lightly as seeds need light to germinate. Place in a warm sunny position. Don't plant out until late spring/early summer, keep moist on transplant. Don't overfeed - likes impoverished soil"
High-quality evidence was found to exist for the use of Galphimia glauca (galphimia) for anxiety disorders [1]Dose: Dried herb 0.6–1 g per day standardized to 0.175–0.348 mg of galphimine B
Clinical trials showing equivalence to synthetic anxiolytics
No adverse reactions found in studiesGeneralized anxiety, GAD
While emerging data is encouraging, further placebo-controlled studies are needed.
Galphimines have been identified as active compounds in galphimia, with the nor-secotriterpenes galphimine A and galphimine B, being shown to have the strongest anxiolytic activity. Galphimine B has been considered the primary active constituent for galphimia’s anxiolytic and sedative effect, and is the constituent standardized for clinical trials. Galphimine B has been shown to interact with serotonergic transmission in the dorsal hippocampus in rats. This occurs by increasing the frequency of neuronal discharge in CA1 cells, resulting in activation of 5HT(1A) receptors. One study in mice demonstrated that galphimines cross the blood–brain barrier, with galphimine A found to have an effect on the central nervous system.
2.5.3 Evidence of Efficacy
2.5.3.1 Preclinical
A number of galphimine constituents, including galphimine B, were evaluated for their anxiolytic effects in mice using the EPM. Mice were intraperitoneally administered 15 mg/kg of a galaphimine derivative 1 hour before testing. An anxiolytic-like effect in the mice was found for both galphimine A and galphimine B, with a significant increase in the time spent in and number of entries into the open arm in the EPM. A second study on mice used a methanolic extract (standardized for galphimine B, 8.3 mg/g) at different doses (125, 250, 500, 1000 and 2000 mg/kg), which were orally administered at three different times (24, 18 and 1 hour before the test). Significant anxiolytic-like effects were found in the light–dark paradigm test and the EPM, but not the forced swimming test.2.5.3.2 Clinical
Two clinical trials have found galphimia to be an effective anxiolytic. The first was a 4-week, positive-controlled double-blind RCT, with a cohort of 152 patients with a DSM-IV diagnosis of GAD and HAMA scores ≥19 . The two groups received either galphimia aqueous extract (310 mg standardized to 0.348 mg of galphimine , or the benzodiazepine lorazepam (1 mg). Each treatment was administered in capsule form (identical in appearance) twice daily. Both groups demonstrated a significant reduction in anxiety symptoms. There were no significant side effects reported in the galphimia group, which contrasted with the lorazepam group, in which over 21 % of people reported excessive sedation.
, or the benzodiazepine lorazepam (1 mg). Each treatment was administered in capsule form (identical in appearance) twice daily. Both groups demonstrated a significant reduction in anxiety symptoms. There were no significant side effects reported in the galphimia group, which contrasted with the lorazepam group, in which over 21 % of people reported excessive sedation. https://neupsykey.com/herbal-anxiolytics-with-sedative-actions/
"0.175 mg of galphimine-B and administered for 15 weeks to patients with generalized anxiety disorder, showed greater anxiolytic effectiveness than that obtained with lorazepam, with high percentages of therapeutic tolerability and safety." [2, 3]
Galphimia glauca has been used for many years in Mexican traditional medicine for treating mental diseases, particularly nervous hyperexcitability disorders. This plant contains galphimines which have been shown to possess the ability of modifying the frequency of discharge of dopaminergic neurons in the Ventral tegmental area [4]. Galphimine-B appears to be an allosteric modulator of 5HT1A receptors [5] It was capable of blocking positive and cognitive symptoms associated with psychosis induced by ketamine [6]
Anti-inflammatory activity and chemical profile of Galphimia glauca.
[1] https://www.ncbi.nlm.nih.gov/pubmed/29575228
[2] https://www.ncbi.nlm.nih.gov/pubmed/22828921
[3] https://www.ncbi.nlm.nih.gov/pubmed/17562493
[4] https://www.ncbi.nlm.nih.gov/pubmed/12567277
[5] https://www.ncbi.nlm.nih.gov/pubmed/21742023
[6] https://www.ncbi.nlm.nih.gov/pubmed/29710504-
 4
4
-
-
I'm not sure about how long SSRI medications induce changes to 5-HT2ARs particularly with relevance to being 'constitutionally right' for tryptamines, mindperformer is likely more versed, but there are some imaging studies with regard to depression. I'd say a lot of the binding potentials change depending on the course of the illness, too? A remitted depression etc being different. More so, binding pattern for 5-HT1A/2A seems to change in depression and might be long term
...findings should be considered preliminary but suggest that recovered subjects with a history of recurrent major depression have elevated binding potential of cortical 5-HT2A receptors. The correlation of increased 5-HT2A receptor binding potential with increased scores on Dysfunctional Attitudes Scale" [1]
Higher 5-HT1A receptor binding potential has been found in major depressive disorder (MDD) during and between major depressive episodes. [2] -
Thanks for your awesome contributions @mindperformer Appreciate the directions to look into and the plants you mention
One I'm currently interested in, drying a bit of material can probably spare some for bioassaysGalphimia (Galphimia glauca)
Dried herb 0.6–1 g per day standardized to 0.175–0.348 mg of galphimine B
Galphimine B
Clinical trials showing equivalence to synthetic anxiolytics
No adverse reactions found in studies
Generalized anxiety, GAD
While emerging data is encouraging, further placebo-controlled studies are needed.Galphimines have been identified as active compounds in galphimia, with the nor-secotriterpenes galphimine A and galphimine B, being shown to have the strongest anxiolytic activity. Galphimine B has been considered the primary active constituent for galphimia’s anxiolytic and sedative effect, and is the constituent standardized for clinical trials. Galphimine B has been shown to interact with serotonergic transmission in the dorsal hippocampus in rats. This occurs by increasing the frequency of neuronal discharge in CA1 cells, resulting in activation of 5HT(1A) receptors. One study in mice demonstrated that galphimines cross the blood–brain barrier, with galphimine A found to have an effect on the central nervous system.
2.5.3 Evidence of Efficacy
2.5.3.1 Preclinical
A number of galphimine constituents, including galphimine B, were evaluated for their anxiolytic effects in mice using the EPM. Mice were intraperitoneally administered 15 mg/kg of a galaphimine derivative 1 hour before testing. An anxiolytic-like effect in the mice was found for both galphimine A and galphimine B, with a significant increase in the time spent in and number of entries into the open arm in the EPM. A second study on mice used a methanolic extract (standardized for galphimine B, 8.3 mg/g) at different doses (125, 250, 500, 1000 and 2000 mg/kg), which were orally administered at three different times (24, 18 and 1 hour before the test). Significant anxiolytic-like effects were found in the light–dark paradigm test and the EPM, but not the forced swimming test.2.5.3.2 Clinical
Two clinical trials have found galphimia to be an effective anxiolytic. The first was a 4-week, positive-controlled double-blind RCT, with a cohort of 152 patients with a DSM-IV diagnosis of GAD and HAMA scores ≥19 . The two groups received either galphimia aqueous extract (310 mg standardized to 0.348 mg of galphimine B), or the benzodiazepine lorazepam (1 mg). Each treatment was administered in capsule form (identical in appearance) twice daily. Both groups demonstrated a significant reduction in anxiety symptoms. There were no significant side effects reported in the galphimia group, which contrasted with the lorazepam group, in which over 21 % of people reported excessive sedation.
High-quality evidence was found to exist for the use of Galphimia glauca (galphimia) for anxiety disorders [1]."0.175 mg of galphimine-B and administered for 15 weeks to patients with generalized anxiety disorder, showed greater anxiolytic effectiveness than that obtained with lorazepam, with high percentages of therapeutic tolerability and safety." [2, 3]
Galphimia glauca has been used for many years in Mexican traditional medicine for treating mental diseases, particularly nervous hyperexcitability disorders. This plant contains galphimines which have been shown to possess the ability of modifying the frequency of discharge of dopaminergic neurons in the ventral tegmental area [4]. Galphimine-B appears to be an allosteric modulator of 5HT1A receptors [5] It was capable of blocking positive and cognitive symptoms associated with psychosis induced by ketamine [6]
The plant yields approx. 0.26% galphimines by the looks of it
[1] https://www.ncbi.nlm.nih.gov/pubmed/29575228
[2] https://www.ncbi.nlm.nih.gov/pubmed/22828921
[3] https://www.ncbi.nlm.nih.gov/pubmed/17562493
[4] https://www.ncbi.nlm.nih.gov/pubmed/12567277
[5] https://www.ncbi.nlm.nih.gov/pubmed/21742023
[6] https://www.ncbi.nlm.nih.gov/pubmed/29710504 -
I put myself on daily probiotic turmeric. Been doing that for a while now. Anyone use it as a brain tonic?

I whip up a couple of strong (20g) turmeric, ginger, black pepper and occasionally saffron probiotic sludges a day
The more probiotic turmeric combos I get into me, the more I see how much I was probably running on likely extreme neuroinflammation. It's a robust shift, some really positive glimpses at something when I mega dose, some days not always feeling wonderful but on the whole small steps that are generally positive, using pretty much all the polyphenol classes and including the turmeric concoctions at a high dose in a good diet. I'm sticking with this, hoping an antidepressant effect becomes apparent..
So far, the most robust improvement I've had is in self-regulation (which was in tatters) buffering to better levels, along with getting sleep (quite a bit of sleep debt built up), more so than mood.
Quite profound is the way these probiotic turmeric combos seem to be modulating aberrant reward related stuff. It's very anti-addictive but at the same time I'm stopping so many locked in behavioural loops that nothing at all left seems rewarding anymore. Push through it, hope I can write some new eudaimonic pathways
Inflammation and mental health:
Research indicates that mood disturbances and psychiatric disorders are closely related to CNS or whole body inflammation [1]. The prevalence of inflammation, measured by one marker only, in the diagnostic groups of psychotic disorders, mood disorders, neurotic disorders and personality disorders was 32%, 21%, 22% and 42%, respectively [2].
'
Inflammation was consistently found to affect basal ganglia and cortical reward and motor circuits to drive reduced motivation and motor activity, as well as anxiety-related brain regions including amygdala, insula and anterior cingulate cortex, which may result from cytokine effects on monoamines and glutamate [3].
Higher levels of inflammation are associated with longitudinal changes in brain function in regions important for cognition [4]. Increasing evidence points toward an involvement of the immune system in MDD pathogenesis. Inflammation can affect monoaminergic and glutamatergic neurotransmission [5]. Negative symptoms of schizophrenia are associated with increased inflammation [6].
Inflammation may at least partly mediate resting state functional connectivity via effects on mesolimbic and mesocortical dopaminergic systems [7]. Inflammatory measures were positively related to striatolimbic resting-state functional connectivity but negatively related to corticostriatal resting-state functional connectivity
Chronically elevated levels of inflammatory markers, for example, are associated with clinical depression, post-traumatic stress disorder (PTSD) and many other psychological and behavioral issues and likewise these conditions often have elevated impulsivity. Inflammatory mediators promote a general trade-off towards focusing on immediate versus delayed outcomes. Inflammation is particularly influential on impulsivity - higher active inflammation – as quantified by plasma levels of IL-6, TNF-α, and white blood cell count – predicted more impulsivity. The relationship remained significant when controlling for factors known to covary with both inflammation and impulsivity [8]
"Better understanding of the outcomes associated with impulsivity of inflammatory origins may yield low-cost interventions that can ameliorate behavioral problems notoriously resistant to current treatment strategies. For example, anti-inflammatory medications may be helpful as adjunct treatments for behavioral disorders related to impulsivity, such as substance abuse or certain mental illnesses."
[1] http://www.dailymail.co.uk/…/Cambridge-psychiatrist-claims-…
[2] https://www.ncbi.nlm.nih.gov/pubmed/29544672
[3] https://www.ncbi.nlm.nih.gov/pubmed/29173175
[4] https://www.ncbi.nlm.nih.gov/pubmed/29304217
[5] https://www.ncbi.nlm.nih.gov/pubmed/29604382
[6] https://www.ncbi.nlm.nih.gov/pubmed/29499967
[7] https://www.ncbi.nlm.nih.gov/pubmed/29689344[8] https://repository.tcu.edu/handle/116099117/20630
More on neuroinflammation
Mental illnesses and ASD seem to be strongly related to neuroinflammation, activation of inflammation in animal models leads to behavioural abnormalities. That said, it is suggested to be at best one cause of depression [1]. Schizophrenia and autism spectrum disorders share core symptoms and overlap in many ways pathologically, mainly by extensive microglial activation and similar behavioural attributes, this microglial activation also extends to brain injuries. The neuroprotective effect of curcumin is mainly mediated by blockade of microglial cell activation [2].
Psychological stress activates inflammation and that this activation would be found to predict the later development of pathology. Social isolation/feeling lonely is associated with systemic inflammation. There is evidence that a range of psychosocial stressors lead to elevated microglial activity [3]. Neuroticism has also been associated with higher levels of inflammatory markers while conscientiousness has been associated with lower inflammatory markers [4].
Chronic neuroinflammation and the loss of neurotrophic factors promotes 'locked in' behavioural inflexibility and promotes the pathogenesis of disorders such as addictions and feeds antisocial personality traits [5]. A multitude of studies support the notion that inflammatory processes form an integral part of the mechanisms precipitating addictions [6].
It appears elevated neuroinflammation is important throughout the cortico-striato-thalamo-cortical circuit of obsessive compulsive disorder, too [7]
See Resident evil: Inflammation and depression
[1] http://www.psychiatrictimes.com/special-reports/introduction-inflammation-connection
[2] https://www.ncbi.nlm.nih.gov/pubmed/18214347
[3] https://www.ncbi.nlm.nih.gov/pubmed/26847047
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4544833/
[5] https://www.ncbi.nlm.nih.gov/pubmed/28810156
[6] https://www.ncbi.nlm.nih.gov/pubmed/29054292
[7] https://www.ncbi.nlm.nih.gov/pubmed/28636705
Microglial activation - a pathological player?Activated pro-inflammatory microglia trigger anxiety- and depressive-like behaviours, mainly by increasing the expression of pro-inflammatory mediators and neurotoxins in stress-sensitive brain regions. Injury, stress, toxic exposures and social stress can induce microglial over-activation [1]
It is proposed M1 and M2 microglia are related to relapse and remission, respectively in psychiatric disorders and diseases [2]. While activated M1 microglia may exacerbate injury by producing neurotoxic substances when overactivated for prolonged times, activated M2 microglia (the anti-inflammatory and tissue-reparative phenotype) protect neighboring cells by removing cell debris and releasing trophic factors for brain repair. Curcumin promoted microglial M2 polarisation and inhibited M1 polarisation.
Long-term depression is a progressive disease and elevated microglial activation and inflammation play a role, it is suggested targeting the inflammatory process is needed to prevent neuroprogression [3].
Our gut microbiota is critical for modulation of the HPA axis and thus the stress response and brain processes such as myelination, neurogenesis and microglial activation and can effectively modulate behaviour and influence psychological processes such as mood and cognition. The gut microbiota is essential for the maintenance of microglia in a healthy functional state, which is necessary for the prevention of neurodevelopmental and neurodegenerative disorders [4].
Microglia have more recently emerged as key players in regulating neuronal network excitability [5] and reward. Activated microglia within reward circuitry result in disruption of dopaminergic signaling and reward behaviour. Activation of microglia by addictive drugs or other causes results in a proinflammatory dominance of the innate immune system, which is then critically synergise on the neurocircuit of reward and dependence [6]. Repeated drug-induced microglial activation produces progressive increases in microglial reactivity, further potentiating the neurobiological consequences of chronic drug use [7]
Even acute inflammation impairs 'theory of mind' (ToM) explaining social-cognitive deficits in people that exhibit low-grade inflammation [8].
Inflammation, Self-Regulation, and Health: An Immunologic Model of Self-Regulatory Failure
Exposure to stress, infection, and disease in early life increases proinflammatory cytokine activity, which decreases an individual’s self-regulatory ability. Poor self-regulation and poor health behaviours, which lead to greater exposure to stress and disease. As these dynamics continue over childhood and adolescence, compounded by social stressors, more stable differences in brain structure and function can develop that ultimately produce persistent impairments in self-regulation in adulthood.
Dysregulated or enhanced neuroinflammation is argued to facilitate the etiology of mental disorders. Immune system activity — especially components of the immune system involved in inflammation — appear to impair numerous facets of self-regulation: inflammatory activity can impair both cognitive and emotional self-regulation. Markers of systemic inflammation have been associated with brain alterations that negatively impact executive function in humans: higher levels of proinflammatory cytokines at baseline predict lower executive function.
Acute inflammatory challenges alter DLPFC response when individuals engage in tasks that require self-control, reduces resting glucose metabolism in the ACC in humans, which is a brain region critically important in self-regulation and reduces functional connectivity between the medial PFC (mPFC) and brain regions involved in mood and emotion. Inflammatory activity impairs sensitivity to reward. Inflammatory activity may impair self-regulation by reducing motivation and may either help or hinder self-regulation by decreasing sensitivity to reward. Inflammation may modulate mesolimbic and mesocortical dopaminergic systems.
"Prolonged or severe stress exposure disrupts homeostatic or ‘healthy’ communication between the CNS and peripheral immune system, shifting immune signaling toward a proinflammatory state. Part of this response includes elevated and prolonged proinflammatory signaling in the CNS that is argued to be linked with stress-related psychiatric disorders."
There is mounting evidence that social stress activates microglial cells in the central nervous system. Microglial activation is positively correlated with psychiatric disorders. Pro-inflammatory cytokines including IL-1β and TNF-α, can reduce the availability of serotonin, dopamine and noradrenaline by increasing the expression and function of reuptake transporters, reducing synthesis or decreasing monoamine precursors and also act on the glutamate pathway and together with astrocytes stimulate the increased release of this neurotransmitter and decreased brain-derived neurotrophic factor, which ultimately leads to excitotoxicity [9]
Elevated pro-inflammatory cytokine levels caused by microglia activation, often induced by social stress, contributes to the development and persistent anxiety-like behaviour [10]
[1] https://www.frontiersin.org/articles/10.3389/fnbeh.2017.00207/full
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4276905/
[3] https://www.karger.com/Article/Abstract/470805.
[4] https://www.wjgnet.com/1007-9327/full/v23/i30/5486.htm
[5] https://www.hindawi.com/journals/np/2013/429815/
[6] https://www.ncbi.nlm.nih.gov/pubmed/22707932
[7] https://www.colorado.edu/lab/bachtell/research/neuroinflammation-and-addiction
[8] https://www.ncbi.nlm.nih.gov/pubmed/29742460
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5660717/
[10] https://www.nature.com/articles/npp2016102Why turmeric?
Turmeric, a source of curcuminoids, including the essential oil containing ar-turmerone [1] is a neuroprotective and neuropharmacological drug. It may be used in neurodegenerative disorders [2] including MS [3], depression etc. Curcumin may be used as an effective and safe modality for treatment in patients with depression, with a better tolerability profile and safety than SSRIs [4]. Patients receiving curcumin showed increased levels of BDNF relative to baseline, whereas patients receiving placebo showed declines relative to baseline but results did not show more distal effects on cognition or clinical symptoms for patients with schizophrenia [5]
Curcumin may increase the concentration of monoamines available to interact with receptors, alleviating depression
Curcumin strongly inhibits inflammatory cytokines like nuclear factor-kappa B, NLRP3 inflammasome, and interleukin-1B. this may help explain its antidepressant activity.There's suggestion that curcumin may be useful for treating human motivational symptoms
The study findings that epigenetically, cooking with/using whole turmeric is superior to using turmeric extract preparations seem to match my experiences - those 'bioavailability enhanced commercial products' or curcumin extracts (even with piperine) just don't personally compare to solid dose of whole turmeric etc IMO. Something about it fermenting in the gut, activity of the volatiles, or high volume of dispersion/absorption of the curcuminoids through using the actual powder, I'm not sure? Particularly fermented with quality probiotics.
Even a curcumin free water turmeric extract has effects on mood . At least 235 compounds, primarily phenolic compounds and terpenoids, have been identified from C. longa. What's interesting about using whole turmeric is curcumin-free turmeric components such as those in a possess numerous biological activities, including neuroprotective, anti-inflammatory, anticancer, and antidiabetic activities. Volatiles like aromatic-turmerone exerts beneficial effects on the brain - inhibiting microglial activation, preventing brain damage caused by neuroinflammation and increasing neural stem cell proliferation . Bisacurone has been identified as another of these components, also with anti-inflammatory effects.
[1] a) https://www.ncbi.nlm.nih.gov/pubmed/28849618
b ) https://www.ncbi.nlm.nih.gov/pubmed/25928248
[2] https://www.ncbi.nlm.nih.gov/pubmed/22742420
[3] https://www.ncbi.nlm.nih.gov/pubmed/29079885
[4] https://www.ncbi.nlm.nih.gov/pubmed/23832433
[5] https://doi.org/10.1016/j.schres.2017.09.046The effect of curcumin on serotonin appeared to be dose-dependent, at high doses curcumin also increased dopamine and to a lesser extent noradrenaline. Additionally, the effect of curcumin on the serotonergic system was possibly related to its interaction with 5-HT1A/1B and 5-HT2C receptors. In studies, regarding behavioural changes; the effect of curcumin was more pronounced than fluoxetine. Curcumin raised brain GSH and reduced brain MDA, TNF-α and IL-6 contents
Importantly, curcumin normalises the levels of dopamine in the frontal cortex of rats and exerts biochemical and morphological effects of the on the PFC and hippocampus. Curcumin enhances the level of neurotrophic factors such as brain derived neurotrophic factor (BDNF)
There have been signs of antidepressant properties through an interaction of curcumin with dopamine receptors and an increase in brain dopamine levels.
Supplementation of curcuminoids to standard antidepressants showed a significant reduction of anxiety and depression in patients with major depressive disorder Moreover, curcumin extracts significantly improved depressive symptoms and demonstrated anxiolytic effects in patients with atypical depression.
There was a significant improvement of sustained attention, working memory tasks, and mood after curcumin treatment.
Curcumin showed a significant reduction in SGA‑induced body weight gain on the rats. It exerts hypoglycemic, antioxidant, antitumor, and anticarcinogenic activities. It also prevents tardive dyskinesia
Why probiotic?Influence of gut microbiota on neuropsychiatric disorders
Got a broad spectrum of probiotics gong on. Along with things like L. plantarum which significantly reduced anxiety-related behaviour and altered GABAergic and serotonergic signaling in the brain, it also ameliorated cognition deficits but also restored ACh and the histopathological features to control group in an AD model, I'm using a lot of L. rhamnosus rich food which has anxiolytic and mood effects: Lactobacillus rhamnosus, can dramatically alter GABA activity in the brains of mice. It reduces stress-induced elevation in stress hormones. Enriching food with Bifidobacterium longum which decreases anxiety and may improve mood among anxious animal models. Lactobacillus casei which cultures appeared to improve mood among those only with a low/depressive mood at baseline. Bifidobacterium animalis which scavenged free radicals and decreased MAO activity.
"The development of the forebrain, esp. the neocortex, in social mammals and ultimately primates and humans depends on correct and timely signals from microbial symbionts—which is disturbed, when the microbiota is absent or disturbed. Likewise when the microbiome is disturbed, there is evidence of increased hypothalamic–pituitary–adrenal (HPA) axis activity in response to acute stress. The immune pathway within the brain–gut–microbiome axis may be a plausible mediator of the effects of this axis on social behaviour"
Recent data provide evidence that related bacterial species can interact specifically with a variety of different neuronal populations. For example some bacteria affects the functioning of CNS neurons in the hippocampus and amygdala, and alter PFC funtioning. They can alter vagal tone, HPA axis activity, neuroinflammation/microglial activation, alter serotonergic transmission, levels of brain-derived neurotrophic factor, NMDA receptor subunit expression, GABAergic signalling and receptor expression etc [ref] There are also links to a role for oxytocin.
Altering the microbiome has been shown to do things like:
-improve mood, but only in those who have poorer mood at baseline and alter anxiety related measures
-reduce cortisol output in response to an acute stressor
-alter brain activity when processing information related to emotional facial expressions
-improvement in sustained attention in healthy older adults
The first clinical trial of probiotics in bipolar disorder found probiotics lowered the rate of rehospitalisation, building on previous research that has found promise for these in depression, anxiety, cognition, and autism
Supplemental probiotics to combat brain-related dysfunction offers a promising approach [1]. Evidence suggests [2] that chronic administration of Lactobacilli and Bifidobacteria strains can have effects on areas of the brain related to emotion, mood, memory, and somatosensory processing - probiotic ingestion attenuates emotional reactions and decreases activity of certain brain regions when measuring brain responses to emotional stimuliAlong with improved depression, anxiety, anger, and anxiety in adults [3], probiotic intake for 4-6 weeks altered neural activity in brain regions that control central processing of emotion and sensation in healthy women but no change in gut microbial composition was detected [4].
In a more recent study, a slight change was detected in the microbiome and [5]:
Probiotics improved self-reported behavioural measures of positive affect and cognitive reactivity
Probiotic administration influenced the behavioral scores for depression and anxiety questionnaires, significantly increasing positive affect and blunting vulnerability to depression in terms of hopelessness and risk aversion
Probiotics improved memory performance and altered brain activation patterns
Probiotic administration for 4 weeks was associated with changes in brain activation patterns in response to emotional memory and emotional decision-making tasks
In major depression, probiotic (Lactobacillus helveticus and Bifidobacterium longum) resulted in an improvement in BDI score compared with placebo whereas no significant effect of prebiotic supplementation (galactooligosaccharide) was seen [6]
“The Social Network” – How the Gut Microbiome Governs Our Social Behaviour
[1] https://www.ncbi.nlm.nih.gov/pubmed/29701810
[2] https://www.ncbi.nlm.nih.gov/pubmed/29698377
[3] https://www.ncbi.nlm.nih.gov/pubmed/20974015
[4] https://www.ncbi.nlm.nih.gov/pubmed/23474283
[5] https://www.tandfonline.com/doi/abs/10.1080/19490976.2018.1460015
[6] https://doi.org/10.1016/j.clnu.2018.04.010There seem to be changes in the microbiota that are associated with substance use [1] across an array of SUDs and eating disorders [2]
Ethanol drastically changes the microbiome and increase in gut permeability and induces a pro-inflammatory responses. Microbiome alterations were shown to be correlated with alcohol use disorder-related symptoms, i.e. craving, depression and anxiety and manipulations in the gut microbiota may affect cocaine-related behaviors (Animals with reduced gut bacteria showed an enhanced sensitivity to cocaine reward and enhanced sensitivity to the locomotor-sensitising effects of repeated cocaine administration [3]) and methamphetamine [4].
There is a strong negative influence of alcohol dependence on gut microbiota [5] and "Intestinal flora between cocaine users and non-cocaine users and have found that cocaine users have a higher mean relative abundance of Bacteroidetes and a lower abundance of Firmicutes than non-users; are more likely to smoke; have a lower mean percentage of body fat; and consume more alcohol than non-users."
Phytonutrients impact the microbiome “eat the rainbow” AND eat prebiotic and probiotic foods" so to do omega-3's: Some of the health-related benefits of omega-3 may be due, in part, to increases in butyrate-producing bacteria.
You can shift the microbiome with probiotics. Some of the other non-LAB are also now available as supplements. Probiotic intake induced an increase in Proteobacteria and in the Clostridiales spp. Patients taking probiotics had an increased numbers of butyrate-producing bacteria, especially Faecalibacterium and Clostridiales spp. Probiotic intervention modulated the fecal concentrations of butyrate in a manner dependent on the initial levels of short-chain fatty acids (SCFAs) [things like live B. bifidum cells affected the relative abundance of dominant taxa in the fecal microbiota and modulated fecal butyrate levels]
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5472629/
[2] https://www.ncbi.nlm.nih.gov/pubmed/28482009
[3] https://www.ncbi.nlm.nih.gov/pubmed/27752130
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5575146/
[5] https://microbiomejournal.biomedcentral.com/.../s40168...Black pepper - more than a spice and bioavailability enhancer...
"During the time of Hippocrates the pepper was used as both a spice for food and as a medicine. The Asian world has long considered black pepper to be an important spice for detoxifying and as an anti-aging compound. It is widely used in different traditional systems of medicine like Ayurvedic and Unani System of medicines"
Black pepper is itself used as an analgesic, antiinflammatory, anticonvulsant, antioxidant, antidepressant and cognitive-enhancing agent. It contains 5-10% pungent acid-amides, with piperine as its main compound and several others, such as the N-isobutylamide guineensine which is a nanomolar inhibitor of cellular uptake of the endocannabinoid anandamide.
Recent studies on the pharmacological actions of piperine have demonstrated its antioxidant activity, antiinflammatory [1] and cognitive-enhancing effect following long-term oral administration. It performed as well as memantine in an Alzheimer's model [2]. It reduces cholinesterase levels and amyloidal plaque formation [3].
It is a potent anti-inflammatory [4].
The antidepressant-like effects might depend on the augmentation of the neurotransmitter synthesis or the reduction of the neurotransmitter reuptake, along with inducing BDNF promoter, increasing brain-derived neurotrophic factor expression in the hippocampus and promoting neurite outgrowth [5,6]. It predominately seems to be mediated via the serotonergic system by enhancing 5-HT content [7]
It exerts anxiolytic effects by GABAergic and nitrergic systems [8]
It exerts anticonvulsant effects [9] due to antioxidant actions, as well as TNF-α reduction, along with effects on inhibitory amino acids and on the GABAergic system [10] and analgesic properties dependent on the opioid system [11]
Piperine pre-treatment time-dependently improves the bioavailability of poylphenols, including flavonoids/green tea catechins and curcumin, through the reversible and selective inhibition of UGTs and SULTs. It also increases the bioavailability of things like ashwagandha, rosmarinic acid and a variety of drugs [12]. Enzymatic inhibition by piperine resulted in increased bioavailability of many drugs and nutrients e.g. amoxicillin, ampicillin, acefotaxime, carbamazepine, ciprofloxacin, norfloxacin, metronidazole, oxytetracyclin, nimesulide, pentobarbitone, phenytoin, resveratrol, beta-carotene, curcumin, gallic acid, tiferron, nevirapine, and sparteine by different types of mechanisms.
Curcuminoids and piperine could inhibit drug metabolism but is "unlikely to result in a clinically significant interaction involving CYP3A, CYP2C9 or the paracetamol conjugation enzymes."
[1] https://www.ncbi.nlm.nih.gov/pubmed/28185326
[2] https://www.ncbi.nlm.nih.gov/pubmed/28939403
[3] https://www.ncbi.nlm.nih.gov/pubmed/26023568
[4] https://www.ncbi.nlm.nih.gov/pubmed/28185326
[5] https://www.ncbi.nlm.nih.gov/pubmed/29063362
[6] https://www.ncbi.nlm.nih.gov/pubmed/17701559
[7] https://www.ncbi.nlm.nih.gov/pubmed/21477634
[8] https://www.ncbi.nlm.nih.gov/pubmed/25149996
[9] https://www.ncbi.nlm.nih.gov/pubmed/28352353
[10] https://www.ncbi.nlm.nih.gov/pubmed/23313550
[11] https://www.ncbi.nlm.nih.gov/pubmed/24388894
[12] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3458266/Ginger:
This itself functions as a bioavailability enhancer.
Ginger has also a broad anti-inflammatory properties and may be useful in auto-immune conditions including MS. Ginger and its constituents, such as 6-gingerol, 6-shogaol, 6-paradol, zingerone, and dehydrozingerone, are effective for ameliorating the neurological symptoms of neurodegenerative conditions.
-
 7
7
-
-
I had an interest in the minerals awhile ago, sorry it's not well referenced, these were just my notes: Didn't get to boron...
A good article from 2007, so it's a bit dated, that covers vitamins and minerals.
For zinc, see https://www.psychologytoday.com/…/201309/zinc-antidepressant
It is an effective SSRI augmentation strategy. In addition, chronic zinc treatment induced increases in both 5-HT1AR protein levels and density of 5-HT1A receptor binding sites, it also increased tissue levels of serotonin metabolite and turnover. On the other hand, DA, DOPAC, HVA tissue levels increased while DOPAC/DA and 3MT/DA decreased in the PFC of rats after chronic zinc treatment. Acute treatment induced increases only in tissue levels of DOPAC, and DOPAC/DA - the antidepressant effects of zinc are mediated in concert with the modulation of the serotonergic system including postsynaptic 5-HT1ARs and allude to a possible involvement of dopaminergic neurotransmission in this action.
Magnesium is a treatment option that may offer great potential for patients with MDD and treatment-resistant depression based on prior work in animals and humans. Combined magnesium and vitamin B6 supplementation reduced anxiety but had no effect when used in isolation. A very small study found benefit from a combination probiotics/magnesium orotate formulation adjuvant administered with SSRIs for treatment resistant depression. See http://evolutionarypsychiatry.blogspot.com.au/…/magnesium-a… and Magnesium and depression: https://www.ncbi.nlm.nih.gov/pubmed/27910808
Selenium
Accumulation of reactive species generated during the normal course of metabolism is highly toxic to biological macromolecules and is a major concern in the pathogenesis of chronic diseases and a significant factor for cognitive decline.
The preferential retention of selenium in the brain suggests that it plays important functions. To date mood is the clearest example of an aspect of psychological functioning that is modified by selenium intake. Five studies have reported that a low selenium intake was associated with poorer mood. The underlying mechanism is unclear although a response to supplementation was found with doses greater than those needed to produce maximal activity of the selenoprotein glutathione peroxidase. Although the functions of many selenoproteins are unknown some play important roles in anti-oxidant mechanisms. Selenium likely plays a role in normal aging, schizophrenia, Parkinson's and Alzheimer's disease.
Selenomethionine enhances stress resistance, is effective in promoting neurogenesis, ameliorates aging indicators, improves the cognitive function of AD mice (rescues spatial learning and memory impairments in aged 3xTg-AD mice via decreasing the level of tau protein and tau hyperphosphorylation) and may be a promising therapeutic option for AD as it decreases the deposition of Aβ and tau hyperphosphorylation.
Selenium affects the cells of the nervous system, and, thus, affects mood: neurotransmitters do not turnover as quickly in Selenium deficient individuals
Low Selenium levels are correlated to depression, anxiety, confusion, and hostility.
Supplementing for 5 weeks with 100 mcg of Selenium, lessened anxiety among patients who participated in a clinical trial.
Hospitalized elderly, cancer, and/or HIV patients reported less anxiety after Selenium was added to their diets
• Even though every aerobic cell is at risk of oxidative damage, the brain is especially vulnerable and this condition is a significant factor for cognitive decline.
• Selenium compounds and selenoproteins exhibited a strong antioxidant role Selenium deficiency or altering the structure or deletion of selenoproteins is associated with severe brain injury.
• Maternal Se status is associated with cognitive ability of the new born. However, the relationship between maternal Se and cognitive ability is not linear (inverted “U”) suggesting both deficiency and excessive Se intake may result in adverse neurobehavioral outcomes.
• Selenium nutrition in the elderly prevents the progression of Alzheimer’s disease, cognitive decline, mood disorder, and depression. However, Se supplementation to healthy individuals with adequate baseline Se with no symptom of mood disorder has not been shown to improve moodSelenium has potential antidepressant- and anxiolytic-like effects and "Se is capable of alleviating inflammatory signaling pathways. Obesity is associated with chronic low-grade inflammation. Depression is also defined as an inflammatory disorder. Inflammatory mediators such as tumor necrosis factor-alpha (TNFα) participate in the progression of depression. They are also obesity-associated parameters. Due to TNFα induced depressive-like behaviors and the positive association between this proinflammatory cytokine and obesity, TNFα-activated signaling pathways and those inhibiting them have recently gained importance as potential targets and therapeutic tools, respectively. More studies are necessary to develop compounds with therapeutic nature against depressive disorders and obesity. PPARγ is an important signaling pathway that occurs at the crossroads of depression and obesity. Se, aside from its anti-inflammatory, anticarcinogenic and antioxidative nature, affects also the way of PPARγ action. Se supplementation or fortification ... will be promising approaches for future hope during the treatment of these diseases."
Chromium
Chromium is antidepressive and may help regulate blood sugar. Chromium supplementation for glucose regulation has shown mixed, modest-sized effects in patients with type 2 diabetes (T2DM). Chromium has the potential to improve insulin, dopamine, and serotonin function, The antidepressant activity has been linked to a major role of the AMPA receptor and participation of NMDA glutamatergic and 5-HT1 and 5-HT2A/C serotonin receptors. Chromium treatment decreases the sensitivity of 5-HT2A receptors
Plasma chromium concentrations were inversely associated with T2DM and pre-DM in Chinese adults [1]. A moderate dose of Cr was associated with improved glycemic control whereas a high dose, while showing some improvement, was not better [2]. Combined chromium and magnesium decreases insulin resistance more effectively than either alone [3]. Cr supplementation showed beneficial effects on blood markers of vascular inflammation, insulin resistance, and oxidative stress compared to placebo [4].
What's the difference between the nicotinate and picolinate? "In a recent investigation conducted at the University of Texas at Austin, a group of healthy, sedentary, obese women was given either chromium picolinate or chromium nicotinate (200 mcg twice a day) for nine weeks, The subjects were divided into four groups: 1) chromium picolinate, 2) chromium picolinate with exercise, 3) chromium nicotinate with exercise, and 4) exercise Plus placebo. Twice-a-week exercise was extensive, involving step aerobics, cycling for 30 minutes and resistance training.
Supplementing with chromium picolinate resulted in statistically significant weight gain (+2.9%), caused by a gain in fat-free mass with a slight gain in fat mass.
Exercise plus chromium nicotinate caused a significant reduction in bodyfat (-1.6%) and a lowered insulin response to an oral glucose load. Exercise by itself or with chromium picolinate didn't significantly affect bodyweight, fat mass or fat-free-mass levels.
This is the first study to show that chromium nicotinate plus exercise can cause a significant decrease in bodyweight with a slight gain in muscle, but study authors didn't suggest a mechanism for this effect. Nonetheless, it would seem that giving chromium picolinate to healthy, obese women is contraindicated for weight loss. Using chromium nicotinate plus exercise, however, may increase the weight loss that normally occurs with regular exercise."
[1] Inverse Association of Plasma Chromium Levels with Newly Diagnosed Type 2 Diabetes: A Case-Control Study. https://www.ncbi.nlm.nih.gov/pubmed/28304331
[2] A Double-Blind, Randomized Pilot Trial of Chromium Picolinate for Overweight Individuals with Binge-Eating Disorder: Effects on Glucose Regulation. https://www.ncbi.nlm.nih.gov/pubmed/27835050
[3] Combined chromium and magnesium decreases insulin resistance more effectively than either alone. https://www.ncbi.nlm.nih.gov/pubmed/27702717
[4] Impact of chromium dinicocysteinate supplementation on inflammation, oxidative stress, and insulin resistance in type 2 diabetic subjects: an exploratory analysis of a randomized, double-blind, placebo-controlled study. https://www.ncbi.nlm.nih.gov/pubmed/27687012For a review, see: Selenium, Vanadium, and Chromium as Micronutrients to Improve Metabolic Syndrome.https://www.ncbi.nlm.nih.gov/pubmed/28197835
-
The taurine is seemingly really useful for the impulsiveness and "feeling in control again" at high doses. It seems to settle the pathology. It does seem to modulate aberrant dopaminergic subcortical stuff subjectively for me, the tics etc.
Added a bit of creatine from today... used it before, mainly with things not so great for mental health. Stick with this, the energetics of my brain seems very disturbed.
Creatine as a treatment for people with SSRI-resistant MDD is suggested [1]. Effects of creatine administration on brain energy metabolism and network organization may partly underlie its efficacy [2]. It targets similar pathways to ketamine [3]. Even a single treatment of creatine or exercise has partial effects as an antidepressant in mice with chronic mild stress-induced depression [4]. Combined creatine and exercise has synergic effects and is more effective than a single treatment.
Dietary supplementation with creatine can improve learning, memory, and mitochondrial function and have important implications for the treatment of diseases affecting memory and energy homeostasis [5].
Supplementation with creatine for 6 weeks is associated with improvement in verbal fluency tests in bipolar disorder [6].
"Oral creatine administration may improve short-term memory and intelligence/reasoning of healthy individuals but its effect on other cognitive domains remains unclear. Findings suggest potential benefit for aging and stressed individuals. Since creatine is safe, future studies should include larger sample sizes. It is imperative that creatine should be tested on patients with dementias or cognitive impairment." [7]
'
[1] https://www.ncbi.nlm.nih.gov/pubmed/26907087
[2] https://www.ncbi.nlm.nih.gov/pubmed/26822799
[3] https://www.ncbi.nlm.nih.gov/pubmed/26660117
[4] https://www.ncbi.nlm.nih.gov/pubmed/27757384
[5] https://www.ncbi.nlm.nih.gov/pubmed/29339557
[6] https://www.ncbi.nlm.nih.gov/pubmed/27890303
[7] https://www.ncbi.nlm.nih.gov/pubmed/29704637 -
I'm guessing this is in reference to non-alkaloid constituents only. Don't have any experiences to add but please keep it to legal soap ingredients
Here's some info on what alcohol could potentially pull in the way of non-alkaloid constituents
"Acacia was referred to as ‘the tree of life’, reflecting its healing nature. Early colonial botanists described medicinal attributes of Acacia species that were known by indigenous Australians"
It is said the biological activities of the Australian Acacia gums were similar to those of Gum Arabic, rich in complex polysaccharides, and that these gums may have potential value as functional human food ingredients. They act as quite effective prebiotics. Neuroprotective effects of Gum Arabic have been established in the ageing brain and ingestion causes significant reduction in BMI and body fat percentage among healthy adult females.
Barks and leaves are the most commonly used parts in all cultures (Australian Aboriginal, African, Asian and Arabs). Other parts used, in decreasing order, are: seeds ≥ gum˃ pods˃ roots ≥ woods˃ flowers ≥ twigs.
Many Australian Acacias are potentially useful in the "treatment of diabetes and neurodegenerative disorders. These Acacia species are rich sources of phenolic antioxidants" but I can't see the phenolic content of the gum
[1] Phytochemical and pharmacological investigations of Australian Acacia: An ethnomedicine-guided bioprospective approach https://researchoutput.csu.edu.au/files/9318404/88453
-
 2
2
-
-
“The Social Network” – How the Gut Microbiome Governs Our Social Behaviour
As I continue, I'm quite a bit into my fermented probiotic, polyphenol laden, omega-3 rich, veggie/herb/greens, vitamin and mineral rich and quality plant protein food and beverage bender with exercise (which includes fermented soy, fermented turmerics etc, most beverages are lacto-fermented etc),
The fermented cabbage intake wasn't enough, nor caps of probiotic, nor more prebiotic food, this time I'm going balls to the wall. One thing I'm keen to observe as I shift the bacteria laden food I'm consuming is not just mood, cognition and anxiety parameters but if it shifts social engagement etc.
I'm noting a few subjective things:
- I feel way less perma-stressed, little less anxious, less fragmented with stress hormone pep. Much less emotional dysregulation
- mood is more stable. More functionally grounded. Feels a bit literally soothing without needed to use soothing plant meds. I'm not chasing non food things to lift my mood. Even caffeine use is less tempting, not so much pep required to lift mood.
- Hunger is down
-people aren't giving me the typical annoying 'bloody humans' feelings that normally arise, normally a large portion of the population tends to give me the sh*ts. There's an emotional approach that feels softer. Not quite prosociality but tending that wayBoth urbanisation and social isolation may alter the microbiome to pathology "Urbanization is on the rise, and environments offering a narrow range of microbial exposures are linked to an increased prevalence of both physical and mental disorders." Urban environments are linked to immunoregulatory deficits - "prospective human and mechanistic animal studies strengthen the idea that an exaggerated immune (re)activity plays a role in the development of mental disorders"
A normal, healthy, and rather non-parasitic microbiota may provide developmental cues that facilitate social behaviour. Socially shared microbiomes could drive the evolution of population-specific mating signals and it has been established common group membership and dietary intake can influence and predict gut microbiota composition. More complex socially driven behaviors can modulate microbiota populations [1].
Animals with an altered microbiome spent significantly less time with a conspecific and did not show the typical preference for a novel mouse when given a choice between a familiar and a novel interaction partner.
A "possible mechanism predisposing those with an urban upbringing, relative to those with a rural upbringing, to develop mental disorders in which inflammation has been identified as a risk factor, is an exaggerated inflammatory response following psychosocial stress exposure. Increased inflammation in urban environments may be due to impaired immunoregulation, which is thought to be dependent, at least in part, on reduced exposure, especially during early life, to microorganisms with which mammals coevolved, as has been proposed by the “biodiversity” hypothesis, “missing-microbes” hypothesis, or “old-friends” hypothesis, which all have been evoked to explain the epidemic of inflammatory disease in urban environments." [2]
We may be so removed from old-friends that it is altering social behaviour and as we spread our urbanicity, be spreading pathology: "social behavior affects the composition of the microbiota and vice-versa and differential expression of RNAs has been observed in cognitive disorders that are associated with altered social behaviour. It is well-documented that microbes can directly target the host's transcriptional regulatory machinery. There are several potential routes for microbes to interact with host cellular function and even behavior and some of these may be mediated by alterations of the epigenetic gene regulation in the brain." [3]
"The development of the forebrain, esp. the neocortex, in social mammals and ultimately primates and humans depends on correct and timely signals from microbial symbionts—which is disturbed, when the microbiota is absent or disturbed. Likewise when the microbiome is disturbed, there is evidence of increased hypothalamic–pituitary–adrenal (HPA) axis activity in response to acute stress. The immune pathway within the brain–gut–microbiome axis may be a plausible mediator of the effects of this axis on social behaviour"
Recent data provide evidence that related bacterial species can interact specifically with a variety of different neuronal populations. For example some bacteria affects the functioning of CNS neurons in the hippocampus and amygdala, and alter PFC funtioning. They can alter vagal tone, HPA axis activity, neuroinflammation/microglial activation, alter serotonergic transmission, levels of brain-derived neurotrophic factor, NMDA receptor subunit expression, GABAergic signalling and receptor expression etc [4] There are links to oxytocin with some Lactobacillus.
Altering the microbiome has been shown to do things like:
-improve mood, but only in those who have poorer mood at baseline and alter anxiety related measures
-reduce cortisol output in response to an acute stressor
-alter brain activity when processing information related to emotional facial expressions
-improvement in sustained attention in healthy older adults[1] http://www.microbiomeinstitute.org/…/social-constructs-and-…
[2] http://www.pnas.org/content/early/2018/04/24/1719866115
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4212686/
[4] https://academic.oup.com/…/doi/10.1093/nutrit/nuy009/4985887The microbiome in addictions
What's also interesting to me particularly is how alterations in the gut microbiota affect pathological reward-related behaviour like the intake of drugs of abuse/alcohol and food etc. There seem to be changes in the microbiota that are associated with substance use [1] across an array of SUDs and eating disorders [2]
Ethanol drastically changes the microbiome and increase in gut permeability and induces a pro-inflammatory responses. Microbiome alterations were shown to be correlated with alcohol use disorder-related symptoms, i.e. craving, depression and anxiety and manipulations in the gut microbiota may affect cocaine-related behaviors (Animals with reduced gut bacteria showed an enhanced sensitivity to cocaine reward and enhanced sensitivity to the locomotor-sensitizing effects of repeated cocaine administration [3]) and methamphetamine [4].
There is a strong negative influence of alcohol dependence on gut microbiota [5] and "Intestinal flora between cocaine users and non-cocaine users and have found that cocaine users have a higher mean relative abundance of Bacteroidetes and a lower abundance of Firmicutes than non-users; are more likely to smoke; have a lower mean percentage of body fat; and consume more alcohol than non-users."
Phytonutrients impact the microbiome “eat the rainbow” AND eat prebiotic and probiotic foods" so to do omega-3's: Some of the health-related benefits of omega-3 may be due, in part, to increases in butyrate-producing bacteria.
You can shift the microbiome with probiotics. Some of the other non-LAB are also now available as supplements. Probiotic intake induced an increase in Proteobacteria and in the Clostridiales spp. Patients taking probiotics had an increased numbers of butyrate-producing bacteria, especially Faecalibacterium and Clostridiales spp. Probiotic intervention modulated the fecal concentrations of butyrate in a manner dependent on the initial levels of short-chain fatty acids (SCFAs) [things like live B. bifidum cells affected the relative abundance of dominant taxa in the fecal microbiota and modulated fecal butyrate levels]
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5472629/
[2] https://www.ncbi.nlm.nih.gov/pubmed/28482009
[3] https://www.ncbi.nlm.nih.gov/pubmed/27752130
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5575146/
[5] https://microbiomejournal.biomedcentral.com/.../s40168... -
Thanks for the input. The Galbulimima bark is one I'm yet to try.
I went away from BCAAs and now for brekky have fermented soy protein. It seems good so far, most mood stabilising protein meal I've noted to get exercise done without needing to get pepped and has the satiating/whole body beneficial proteins and hypothetically the encrypted proteins with antidepressant, opioid and cognitive benefits etc with a good level of free aromatic aminos.
Occasionally have a bit of acetyl-L-carnitine. Found my stress responses have gone down since I upped the probiotic food and such seems just as good a stress buffer, to the point where L-lysine/arginine blends weren't needed.
Went back to taurine - why?Taurine and the brain, does it help give you those wings? - I've wondered why they put it in energy drinks etc? There's some suggestion taurine enhances exercise performance, supporting healthy VO2 max, exercise time to exhaustion and maximal workload but does it have much effect on the mind without heaps of caffeine in the mix? I've tried supposedly 'more active' homotaurine derivatives which are supposedly CNS active to not much effect. How much does this often considered to be pretty inert and boring compound do in the brain at high doses, for a reasonable time? Particularly, does it have therapeutic applications?
Seeing it's such a cheap, safe thing that's found to have good effect in psychiatric conditions in some studies [1,2], I've been heaping taurine into my diet, not expecting really anything. There's something very 'modulatory' about it at high dose. I always dismissed it as pretty inert but they're even suggesting it as an option for ADHD. I stopped for a bit and things went a bit downhill.
Taurine effects include: neuromodulatory, osmoregulatory, membrane stabilisation, and antioxidant action coupled with neuroprotective (taurine is a potential therapeutic agent for neurodegenerative diseases, promoting neuronal proliferation, stem cell proliferation, and differentiation, via several mechanisms), anti-diabetic (it improved glucagon activity, promoted glycemic stability, modified glucose levels, successfully addressed hyperglycemia via advanced glycation end-product control, improved insulin secretion and had a beneficial effect on insulin resistance) and anti-depressive effects (regulation of hypothalamic-pituitary-adrenal (HPA) axis and the promotion of neurogenesis, neuronal survival and growth in the hippocampus).
"Dysregulation of dopamine (DA) level has been associated with various psychiatric disorders...
Taurine is a ubiquitous β-amine acid in mammals, which is involved in a variety of physiological and biological processes such as cell membrane stabilization, osmoregulation, detoxification, immune regulation, antioxidation, and neuromodulation. In recent decades, considerable attention has been paid to the role of taurine in the central nervous system. Notably, various evidences have shown that taurine is a neurotransmitter. Taurine has neuroprotective effects and a taurine additive has been suggested as a potential candidate for neuroprotectants. Recent results reported that high-dose taurine improves hyperactive behaviour and brain functional signals
Low-dose taurine favors impulsive behavior and striatal dopamine uptake whereas high-dose taurine improves spatial learning, memory and striatal dopamine uptake.
Supplementation of taurine could be a remedy for ADHD. Since high-dose taurine is non-toxic to humans and has been clinically used to treat various disorders, the findings in this study by using high-dose taurine (560 mg/ 100 g diet) did provide a rational suggestion for high-dose taurine on ADHD treatment.
Notably, much evidence indicates that taurine strengthens the effects of dopamine and has a synergistic effect with dopamine in the brain, inhibiting the reduction of sucrose consumption and improving the learning ability and spatial memory of rats that are exposed to chronic unpredictable mild stress (CUMS)" [3]
Taurine is a psychopharmacologically active compound with potential for "a variety of therapeutic uses including as a neuro-protective, anti-cataleptic, anti-addicting, and analgesic agent."
With regard to the dopamine elevating properties of alcohol, raised levels of taurine in the nucleus accumbens (nAc) is pivotal. Acute or chronic administration of psychotropic drug cocaine may increase extracellular release of endogenous taurine [4]
[1] https://www.ncbi.nlm.nih.gov/pubmed/29561067
[2] https://www.ncbi.nlm.nih.gov/pubmed/27835719
[3] https://www.ncbi.nlm.nih.gov/pubmed/29694913
[4] https://www.ncbi.nlm.nih.gov/pubmed/23392920 -
More lacto-fermenting teas, even some UV experiments at potential photoconversion. Enjoyed the fermented Hibiscus, Spearmint, Ashwagandha lacto-brews etc.
Got some energy to do some experimenting. Thought I'd do some chamomile with a L. plantarum containing starter. Done my turmeric, ginger, Matcha and black pepper. Also done some Kudzu isoflavones with a broad spectrum culture. Trying Heimia at the moment
The microbial fermentation of phytochemicals can be applied in diverse ways to enhance the medicines of plants. I've mentioned the benefits of fermented turmeric and many polyphenols
Although apigenin is the major flavonoid in chamomile, various other phytochemicals also coexist in chamomile extract could be bioconverted and/or hydrolysed to have higher bioactivities. It has improved polyphenol profiles, antioxidative and cytotoxic activities and may be a superior medicine [1]
Chamomile
This ferments really nicely...In the past I would have gone phht at the concept of chamomile intoxication, or it ranking as a feasible interesting psychotropic for clinical level use. Probiotic chamomile tea sounds like the hippiest granny health tonic... out of all the lacto-fermentations so far, it the scariest potent one I've come across, blend that with some stuff and literally knock out potential IMO. Have to do more experimentation...
Apigenin containing plants like chamomile are interesting as it's not just a GABAA modulator, it has been shown to have antidiabetic (this has been recently popular news [1]) , anti-cancer, anti-inflammatory and neuroprotective properties in a number of cell and animal models [2]. It's also showing antidepressant effects [3,4] Apigenin is a ligand for the central benzodiazepine receptors exerting anxiolytic and slight sedative effects (competitively inhibited the binding of flunitrazepam with a Ki of 4 microM)
There's notable effects at pushing the dose of plain chamomile for me, more anxiolytic than getting smashed (lightweights can sometimes relate to simple chamomile tea, I can't). Interestingly, the lacto-fermented chamomile seems to knock me much more than normal high dose chamomile, haven't had a chamomile experience as strong as the lacto-fermented one before... almost concerned at how strong it was vs normal. It's likely the bacteria hydrolyse the flavonoid glycosides in chamomile etc [5] but there could be something more funky.
I've never tried pure apigenin but flavonoids may also be metabolised by the resident microbiota and the resulting products may have greater bioactivity, which differs from that of the parent compounds. The bacterial degradation of flavonols and flavones starts with the reduction of the C2-C3 double bond yielding the corresponding flavanonols and flavanones. In general, flavanones have shown little or no activity in benzodiazepine-binding studies [6]. Apigenin may partly convert into naringenin, which "does not produce anxiolysis by modulation of the GABAA receptor; however, the findings indicate that naringenin decreases motor movements" What a spectrum of fermentation microbes does is a good question.
[1] https://www.independent.co.uk/…/camomile-tea-diabetes-contr…
[2] https://www.nature.com/articles/srep31450
[3] https://www.ncbi.nlm.nih.gov/pubmed/26416673
[4] https://www.ncbi.nlm.nih.gov/pubmed/26826594
[5] https://www.tandfonline.com/…/full/10…/19490976.2016.1158395
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3087128/Heimia:
Heimia is a nice tea, an attunement to relate to I find but is there something that brings out the medicinal aspects that the traditional use alludes to that we haven't quite got right for optimal effects?
Some of the more experienced people get an opaque milky sun fermented tea, that's the medicine they relate to. That makes me wonder if they are inducing some kind of (bacterial/yeast) bioconversion in their fermentation. Even as a clearer tea that's sun exposed for a day, I find it nice. Good flavours. Nice bit of meditativeish effect. Feeling of more that things are "OK".
I want to see what providing some other conditions does to Heimia.
I've got two batches, one I'm going to sun-expose and lacto-ferment with broad-spectrum probiotic strains. It's possible that the alkaloids will bioconvert and highly likely the polyphenols will...
The other, I'm going to UV irradiate @254nm for some time, see if there's a UV conversion/some kind of photoisomerisation etc that takes place, hence the reason for using sun fermentation.
Using 80g/L Heimia - mainly stem.
This didn't develop the same taste as sun fermented... much milder flavour.
@equivalent 10g dry "shamanic inititiation dose" on just diet and exercise, after a bit of time, it feels seemingly on par with more traditionally sun fermented material at the same dose, light mellow relaxation with enhanced 'presence' so far. Nice walk in the sun.
Wouldn't say it's uncovered anything different effect wise nor a drastic potency increase that warrants using UV, from initial impressions.
@20g, the walk was "much more interesting" in the moonlight, saturation of being in the moment, somewhat anxiolytic, soaking up the presentBy day 4 this is a nice cloudy lacto-tea brew.KudzuKudzu is said to be a nervine, promoting feelings of well-being, it is said to have soothing effects, combat excessive stress and helps create a relaxed mood to work with emotions. Getting back to splashing around standardised extract in the diet.
With Kudzu, which has puerarin as the main isoflavone glycoside (8-C-glucoside of daidzein), fermented Pueraria radix might be more effective than non-fermented versions [2] and can be useful as a functional food. Kudzu root in the diet is associated with a decrease in fasting glucose and improvements in both glucose tolerance (oral glucose tolerance test) as well as insulin tolerance (indicative of insulin sensitivity) [3].
Lactobacillus strains facilitate the conversion of isoflavone glycosides (daidzin, genistin) into bioactive aglycones (daidzein, genistein) and this is used in traditional oriental medicine systems [4]. Dihydrogenistein and dihydrodaidzein are produced by Lactobacillus rhamnosus [5] and some Lactobacillus strains create equol [6].
When given orally, daidzein, daidzin, and puerarin decreased ethanol intake by 75%, 50%, and 40% so optimising diadzein concentration and other isoflavones may be promising [7]. While daidzin in vitro is a strong, selective and reversible inhibitor of aldehyde dehydrogenase which is promising for many addictions from alcohol to cocaine, the other constituents may also act on the CNS receptor gene expression through the opioid system, exhibiting antagonist activity by influencing the opioid receptors mu, delta and the expression of endogenous opioid precursors (proopiomelanocortin) [8] The reversal of alcohol preference produced by these compounds may be mediated via the CNS and converting to more CNS active and permeable isoflavones may enhance the antiaddictive potential.
Puerarin-related compounds have strong preclinical support in favour of use in neurodegenerative diseases, partly through ERβ. The actives modulate neurotransmitter levels [9]. Equol is potent in attenuating microglial activation and potentiates neuroprotection [10].
[1] https://dx.doi.org/10.1631%2Fjzus.B1600063
[2] https://scialert.net/fulltext/?doi=ajava.2014.556.567
[3] https://www.ncbi.nlm.nih.gov/pubmed/23123226
[4] https://link.springer.com/artic…/10.1007%2Fs12257-012-0073-7
[5] https://www.ncbi.nlm.nih.gov/pubmed/29081087
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5813953/
[7] https://www.ncbi.nlm.nih.gov/pubmed/8800381
[8] https://www.ncbi.nlm.nih.gov/pubmed/24501814
[9] https://www.ncbi.nlm.nih.gov/pubmed/28928659
[10] https://www.ncbi.nlm.nih.gov/pubmed/28264445Fermenting protein
Bioactive Molecules Released in Food by Lactic Acid Bacteria: Encrypted Peptides and Biogenic Amines
Who's eaten fermented soy protein products to a good degree? Do they have CNS effects you can pick up, mainly looking towards feelings of anxiolysis, vs other proteins? Not just on the potential phytoestrogenic actions of the fermented isoflavones in less refined fermented soy, but the feeling of the protein, what do you think of it?
Proteins: Soy and maybe Hemp - I have this totally bland soy protein, I want to ferment it... anyone seen a recipe for making a tasty fermented soy protein drink?
Normally, enzymatic hydrolysis or fermentation is used to enhance the functionality of protein ingredients, which may lead to the production of short peptide sequences with various bioactivities. Many experimental evidences demonstrate that some LAB strains also produce anti-hypertensive, anti-thrombotic, cholesterol-lowering, metal-chelating, antimicrobial, anti-oxidant, immune-modulating, chaperone-like and opioid/opioid antagonist peptides from food proteins
Fermenting soy liberates opioid peptides (i.e., soymorphins-5,-6, and -7, and rubiscolin-5 and -6, respectively), displaying anxiolytic effects, food intake controlling action and enhancement of memory, have been described. These are produced by LAB proteolytic action toward soy betaconglycinine. These are similar to the β-casomorphins
While I didn't find Lactium interesting, it is αS1-casein tryptic hydrolysate containing bioactive decapeptides that act on GABA receptors. Lactium (150 mg/day) may be helpful in reducing stress and stress associated symptoms promote relaxation and can be useful.
There are neuromodulating peptides found from degrading β-conglycinin that extend beyond opioid peptides.
Fermentation on soy protein increases digestability and changes the protein microstructure [1]. Fermentation increases the number of small bioactive peptides and free amino acids (AA)
"Studies on the favorable effects of soy products have indicated that the effects are mostly exerted by the protein itself although isoflavones contained in an isolated soy protein fraction might make a minimal contribution to these effects. A number of animal and human studies showed that β-conglycinin, when compared with milk protein (casein), has anti-atherosclerotic, serum triglyceride-reducing, cholesterol-lowering, and anti-obesity effects" [2]
There's potential for optimising things like:
-the soymorphins and rubiscolins, displaying anxiolytic effects, food intake controlling action and enhancement of memory as mentioned earlier
- Orally active decapeptides like soy-deprestatin, which exhibited antidepressant-like effects at a dose of 0.3 mg/kg via a novel pathway mediated by 5-HT1A, followed by D1 and GABAA systems [3]
- dopaminergic undecapeptides [4]
- Exogenous ghrelin-releasing peptides [5]
- anti-cancer and anti-inflammatory effects have been suggested for some protein hydrolysates
β-conglycinin is itself interesting for those without aversion to soy - it improves carbohydrate and lipid metabolism, exerting hypolipidemic effects through an acceleration in carbohydrate consumption associated with an increase in adiponectin in rats [6]. β-conglycinin may increasing insulin sensitivity, regulating lipid metabolism, improving renal function markers, and inhibit ACE activity in diabetes [7]
[1] https://www.ncbi.nlm.nih.gov/pubmed/28975646
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4911586/
[3] https://www.ncbi.nlm.nih.gov/pubmed/28970253
[4] https://www.ncbi.nlm.nih.gov/pubmed/29577906
[5] https://www.ncbi.nlm.nih.gov/pubmed/27416956
[6] https://www.ncbi.nlm.nih.gov/pubmed/25913002
[7] https://www.ncbi.nlm.nih.gov/pubmed/25205218I haven't seen fermented Hemp?
Also want to ferment omega-3's into the protein blend, these lactoferment beneficially


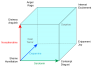





Modulating 5-HT - dietary augmentation interventions
in Pharmacology, Chemistry & Medicine
Posted · Edited by Alchemica
The recent dietary modification has given me baseline stable state where it feels feasible to attempt simple meditations, started that and try and incorporate that each morning, whereas before the dysregulation was something I couldn't at all over-ride.
In SUDs, there is a brain-state shift from a hippocampal and PFC- mediated regulatory state to a more primitive and dysregulated amygdala and insula-mediated state underlying emotion dysregulation
Few things I've noticed:
Trp influences behaviour along the agonistic–affiliative axis, it regulates the tone of interactions along the axis that runs from agreeable to quarrelsome to overt aggression.
Tryptophan
- promotes prosocial behaviour.
- promotes interpersonal trust.
- causes greater sharing and helpfulness, greater perspective taking and emotion recognition.
- improves control over antisocial behaviour - It allows regulation of aggression and positive social interactions, as well as emotional processing
Serotonergic signalling impacts the two-way interaction between each of the following pairs: mood and social behaviour, mood and cognition, social behaviour and cognition and increases prosocial behaviours
- Enhanced serotonergic function might promote effortful control over underlying action tendencies
- Enhancing serotonergic function should decrease reliance on habitual, reflexive forms of self-regulation and increase the use of effortful, reflective forms of behaviour regulation
- Enhanced 5-HT leads to blunted evaluative responses to both positive and negative stimuli
Manipulations of serotonergic tone affect reward [1] and decision making [2]. Depleted states cause one to be significantly more perseverative over choices and (acutely) significantly less sensitive to reward (lower reward magnitude)
For me, the impulsive reward chasing loops start to seemingly undergo some changes (serotonin has been proposed as a possible encoder of reward and facilitator of reward extinction): you go from impulsive action to greater conscious choice but it doesn't feel as impulsively rewarding to do things. It feels a little blunting. So those healthy addictions, for me gardening and daily walking, start to feel more effort-driven than impulse driven and require more effort in. If you're not careful, you can become content with inaction.
Depletion of 5-HT enhances behavioural and brain responsiveness to aversive signals, while disinhibiting previously rewarded but now aversive behaviours [3]. Dysfunction by the serotonergic system in impulse control disorders reflect inhibitory impairment of the prefrontal cortex [4].
You want 'better'. It has been proposed "5-HT encodes beneficialness, and may signal motivation to either maintain or switch current behaviour, for example displayed by 5-HT’s role in facilitating patience for future rewards"
[1] https://www.frontiersin.org/articles/…/fnhum.2017.00484/full
[2] http://www.jneurosci.org/content/32/17/5833
[3] https://www.ncbi.nlm.nih.gov/pubmed/18069045
[4] http://europepmc.org/articles/PMC4117279
Imagine, after a long time of not knowing/feeling emotions or self-regulating them, you are now unable to avoid the blunt edges of tough emotions which are, after so long, alien influences. Sadness, anger, disappointment, frustration, boredom, annoyance, confusion, disgust, surprise, anxiety, guilt, shame, embarrassment. There is no more avoidance. Your escape route has gone. ‘Feeling all the feels’ is like being on a furious roller coaster, particularly when your emotional regulation route has always been psychopharmacological.
There's not just the array of problems induced by self-medication but also over a decade of often supratherapeutic doses of potent psychotropics/ECT, including over neurodevelopmentally-sensitive timeframes when the prefrontal networks and skills in emotional regulation should have been developing.
I'll attest that attempting meditation when all emotional regulation is in tatters and you have pure negative affect is plain frustrating, studies show that greater intact emotional regulation when meditating produces more benefits in affect regulation
You can use attentional bias modification: mindfully focus on their breath, or on emotions. Breathing meditation and emotion-focused meditation may constitute effective emotion regulation strategies to deal with negatively valenced emotional states [1]
Short meditation [2] enhanced mood (i.e., total mood disturbance, anxiety, and fatigue), cognition (i.e., attention, working memory, and recognition memory), and improved the response to acute stress
Simple 13 min meditation [they used Journey Meditation (http://www.journeymeditation.com/) for 8 weeks has been studied. 8 weeks of brief daily meditation relieves feelings of negativity by decreasing levels of mood disturbance. It exhibited a similar range of cognitive benefits as the effects previously reported following longer duration, more intense meditation training
If you get through regulating and managing persistent negative emotion, you start to feel the good ones in all their glory too. All of the lovely positive emotions such as; satisfaction, joy, elation, excitement, love, contentment, gratitude, hope, amusement, inspiration, awe, interest.
[1] https://www.ncbi.nlm.nih.gov/pubmed/30146138
[2] https://www.ncbi.nlm.nih.gov/pubmed/30153464
The world of emotions
Key to this employment of equanimity to reduce emotional reactivity is the intentional cultivation of awareness towards emotional information. I was shutting down that world.
"Limiting cognitive elaboration in favor of momentary awareness appears to reduce automatic negative self-evaluation, increase tolerance for negative affect and pain, and help to engender self-compassion and empathy in chronically dysphoric individuals" [1] - cognitive elaboration often automatically triggers negative self-judgments that cannot be voluntarily overridden
"Dysregulation of fronto-limbic control regions may lead to maladaptive, ruminative, and egocentric attention contributing to depressive affect. In mood disorders, cognitive control appears to be impaired, there is compromised connectivity between the PFC and limbic regions such as the amygdala. Thus, activating PFC regions in efforts to reappraise negative feelings may backfire, bringing attention to focus on dysphoric mood without a commensurate reduction in the intensity of negative feelings."
Instead, you begin observing, describing, acting with awareness, being nonreactive, and being nonjudging. When emotional information is consciously attended, you evoke less of an amygdala response and engaged greater prefrontal cortical resources.
By deploying attentional resources to recruit a network that limits habitual elaboration and self-referential narrative "automatic recruitment of temporally-extended, self-referential narrative generation may undergo a form of neural extinction, restoring autonomy to the central executive system and freeing it from its habitual applications
For me, some of the skills I'm trying to bolster are:
1. Acceptance of emotional responses (ACCEPTANCE)
2. Engaging in goal directed behavior (GOALS)
3. Impulse control (IMPULSE)
4. Emotional awareness (AWARENESS)
5. Emotion regulation strategies (STRATEGIES)
Mindful emotion regulation can be construed as a process of ‘turning toward’ momentary experience - attention is positively directed towards present moment sensation, providing a non-conceptual and non-threatening focus for attention
6. Emotional clarity (CLARITY)
Improving the self-regulation of attention might reduce the negative emotionality associated with ruminative thought patterns and the tendency to suppress thoughts, both of which have been associated with craving and relapse in addictive behaviours [2]
The development of an attitude of acceptance (i.e. a nonjudging/nonattached view of experiences) could reduce negativity affectivity by reinforcing distress tolerance abilities in relation to several experiences (e.g. craving, stress, anxiety)
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3303604/
[2] https://www.ncbi.nlm.nih.gov/pubmed/30216741
Tryptophan and ASD
I always had strong affinity for serotonergics but addressing it at the dietary level is so much more sustainably promising for me than other approaches. Trp, B-vitamins and magnesium have been used.
While radically boosting prosociality through empathogens is being researched for autism, I feel it often needs to be addressed at a more fundamental and sustainable level. A slow and steady, easily integratable and sustainable induction of mood, emotion and greater prosociality can seemingly be had through safer dietary serotonergic interventions.
"Low brain tryptophan availability… could be one of the possible mechanisms involved in the alteration of serotonergic function in autism.”
"Serotonergic abnormalities were reported in ASD. Research indicates that the reduced levels of serotonin are correlated with the occurrence of impulsive and aggressive behavior, fatigue, depression episodes, insomnia and increased sensitivity to pain. There is evidence that pharmacological treatment is aiming the reduction of the serotonergic neurotransmission results in worsening of autistic symptoms" [1]
"Often, families observe that anxiety and subsequent frustration leading to aggression can be better controlled by administering this supplement on a daily basis.
Likewise, more focus and attention may accompany administration of tryptophan" [2]
It seems to have quite prominent socio-emotional qualities in the way I'm using it that have not really been researched in ASD
"BDNF and tryptophan metabolism appear to take part in the pathophysiology of autism spectrum disorders and their phenotypes." [3] Lower tryptophan and KA levels were characteristics of both childhood autism and intellectual disability disorder. Lower 5-HT synthesis were hallmarks of AS
[1] https://link.springer.com/article/10.1007/s11011-017-0045-x
[2] http://www.theautismdoctor.com/tryptophan-to-treat-autism/
[3] https://www.ncbi.nlm.nih.gov/pubmed/30033880
It also targets another issue for me:
Recent findings suggested the serotonin system may be an effective target for prevention and treatment of mild cognitive impairment
“Now that we have more evidence that serotonin is a chemical that appears affected early in cognitive decline, we suspect that increasing serotonin function in the brain could prevent memory loss from getting worse and slow disease progression.”
Researchers have tried with limited success to treat Alzheimer’s disease and cognitive impairment with antidepressants such as SSRIs
What if it's as simple as tryptophan as a starter? I was skeptical about simple tryptophan, assuming it could worsen pathology through often noted disturbed tryptophan metabolism.
L-Tryptophan (TrP) enriched diet protect against memory deficits during physiological aging
5-HT modulates BDNF mRNA levels. TrP significantly elevates the number of 5-HT immunoreactive fibers and this correlated with BDNF increase in the FC and hippocampal region
"...enhanced TrP intake and the consequent increase in 5-HT neurotransmission may act as a modulator of BDNF system suggesting a possible mechanism for the protective role of serotonergic system on memory impairment occurring along normal aging process." [1]
"data suggest that enhanced TrP intake, and in consequence a potential increase in 5-HT neurotransmission, might be beneficial in preventing age-related detrimental features by inhibition of hippocampal apoptosis." [2]
https://www.healio.com/.../serotonin-may-play-important...
[1] https://www.ncbi.nlm.nih.gov/pubmed/26444078
[2] https://www.ncbi.nlm.nih.gov/pubmed/27889579
Targeting alexithymia